Part 2 of a series designed to raise awareness of breathing problems and the procedures currently available to orthodontists to assist patients in improving their breathing, sleeping, and overall health
By Robert “Tito” Norris, DDS
In an article in the July/August 2024 issue of Orthodontic Products, signs and symptoms of airway issues were discussed. The importance of having every new patient complete a sleep questionnaire was emphasized, and the possible sources of nasopharyngeal obstruction were reviewed. It also explained why it is of the utmost importance when treating patients with airway obstruction(s) to develop a relationship with a progressive ear, nose, and throat (ENT) physician, as appropriate referrals can not only help identify the specific cause(s) of airway obstruction but also a progressive (ENT) physician can utilize any number of procedures to aid in the removal or reduction of obstructions.
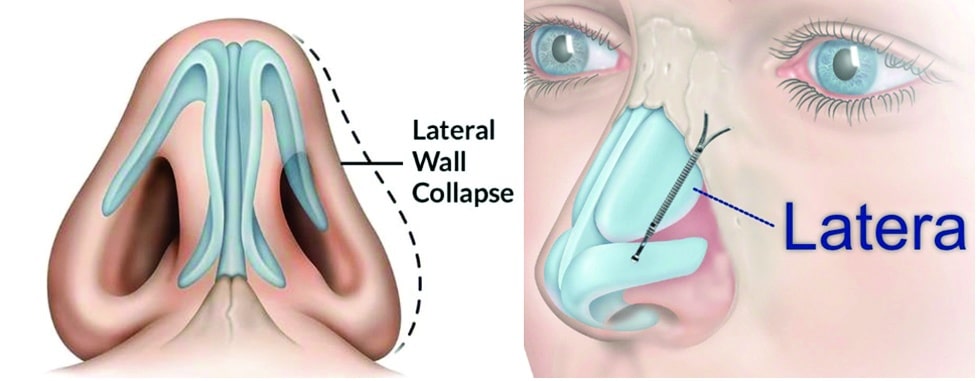
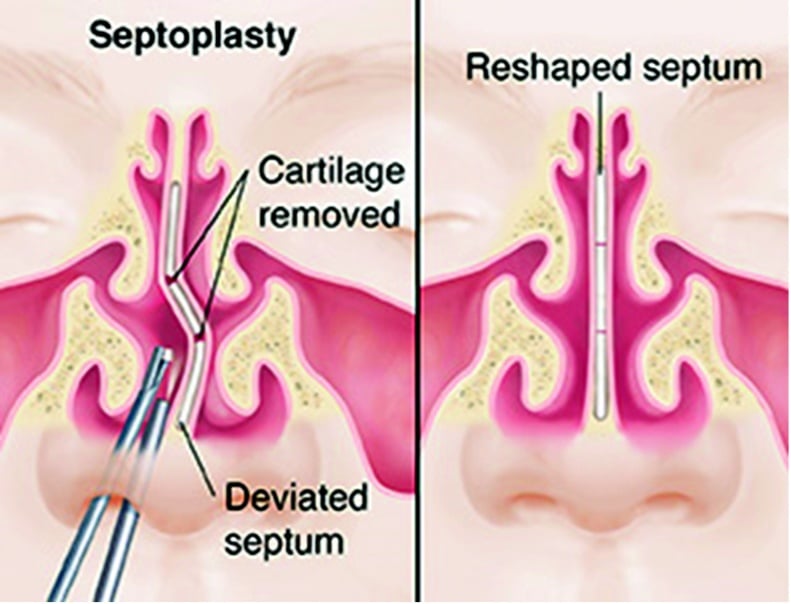
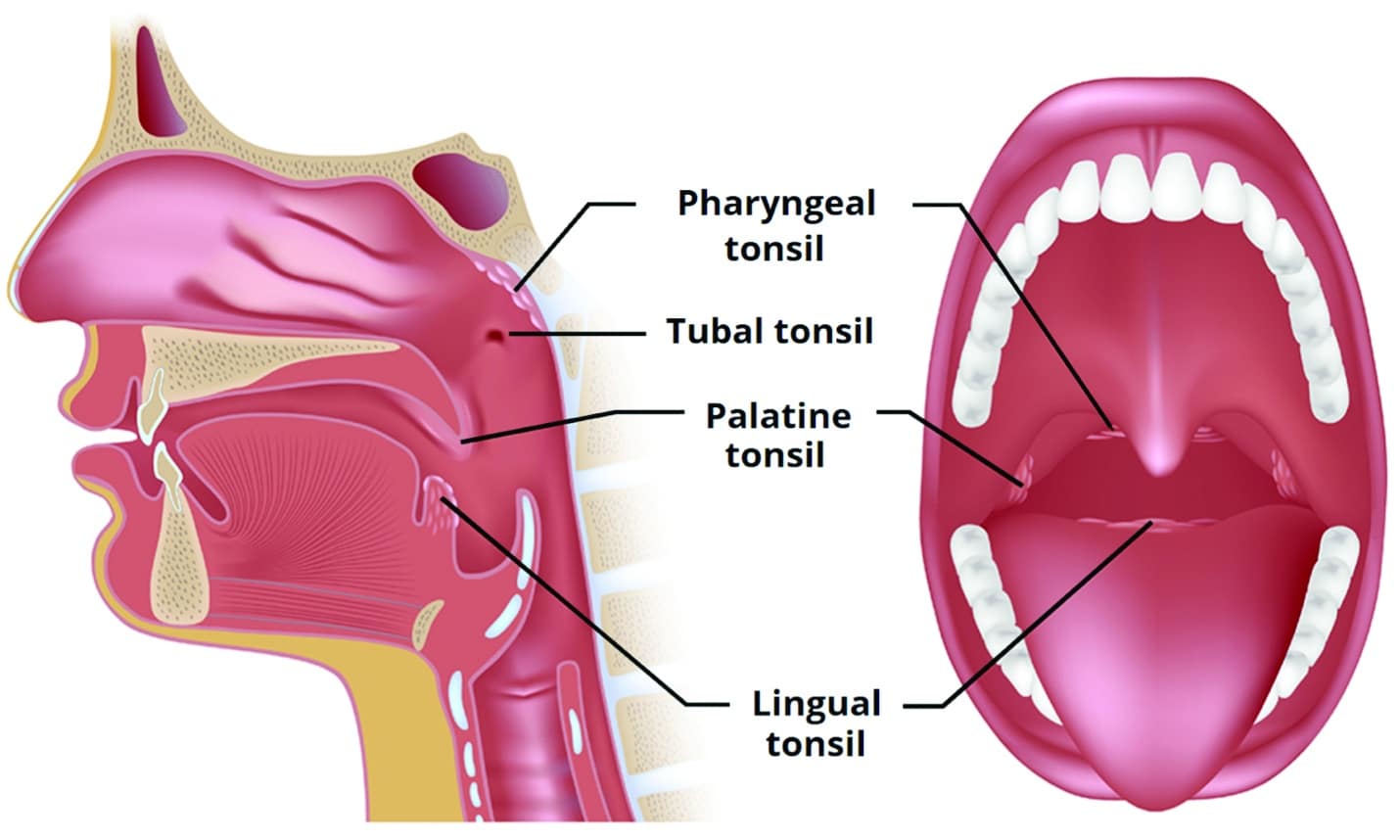
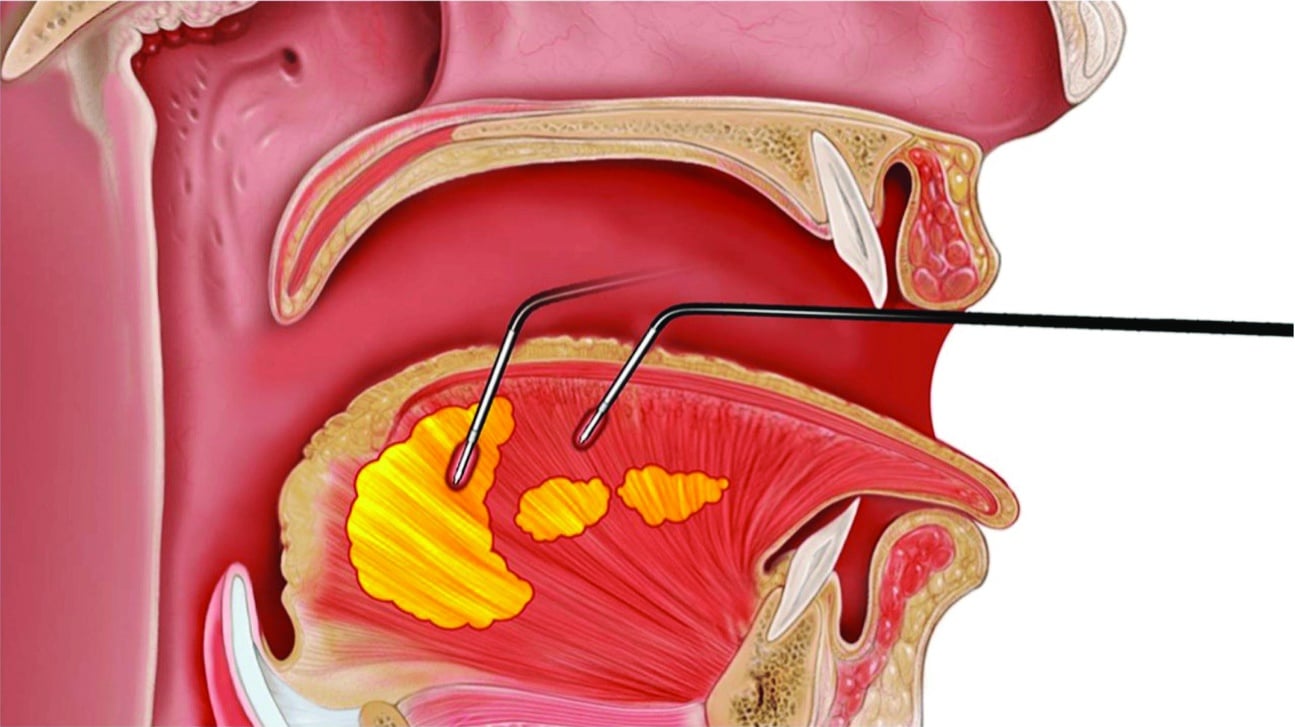
Examples of procedures performed by ENT physicians include cartilaginous spreader grafts, radio-ablation, and synthetic stents to help correct nasal valve collapse (Figure 1). A deviated septum can be surgically corrected (Figure 2), and turbinates can be reduced via surgical resection or radio-ablation. A tonsillotomy or tonsillectomy can be performed at the adenoid/pharyngeal, palatine, and/or lingual tonsillar level (Figure 3). The tongue volume can also be reduced via resection or radio-ablation (Figure 4). A uvulopalatopharyngoplasty (UPPP) can also be indicated on certain patients with excessive or flaccid throat tissues.
The orthodontist’s role in expanding the airways
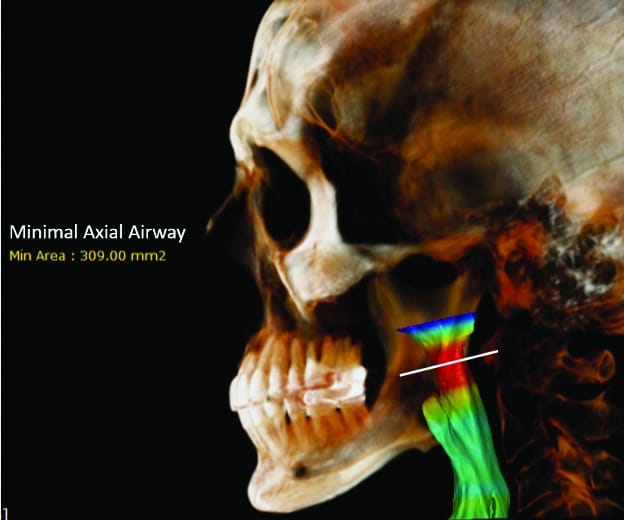
While the procedures performed by ENT surgeons are subtractive in nature, orthodontists are uniquely positioned to expand nasal and pharyngeal airways. By increasing the size of the oral cavity, the volume of the tongue can be shifted from the posterior pharyngeal airway space into the larger oral cavity, thus improving the minimal axial airway (MAA) of the oropharynx (Figure 5). Expansion of the oral cavity can be achieved in two ways: dentoalveolar expansion and skeletal expansion.
Dentoalveolar expansion
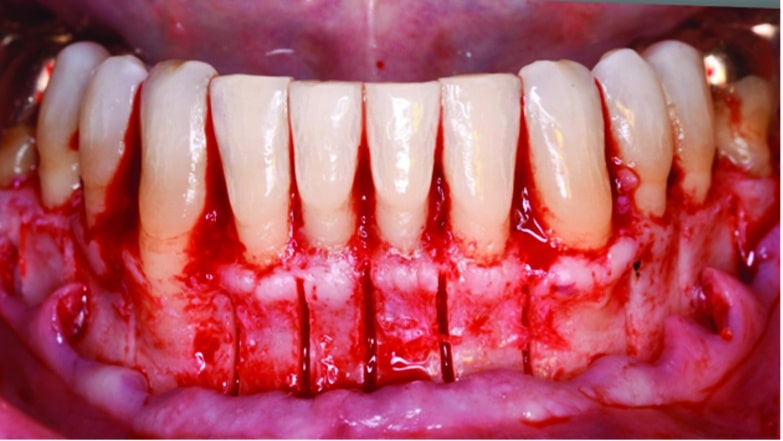
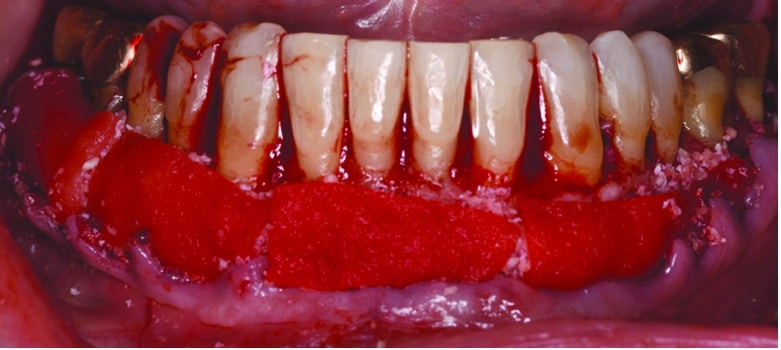
Dentoalveolar expansion consists of broadening the teeth within the confines of the alveolar housing of bone. This type of expansion can be achieved transversely as well as anteroposteriorly, using traditional wires and brackets as well as aligners. The amount of dentoalveolar expansion is limited by the thickness of facial bone and soft tissue into which the teeth can be moved. However, there are adjunctive surgical procedures, such as Surgically Assisted Orthodontic Treatment (SFOT) aka Periodontally Assisted Orthodontics (PAO) aka Wilckodontics, which can augment the facial bone and gingiva, thus increasing the magnitude of dentoalveolar expansion (Figure 6).
Skeletal expansion
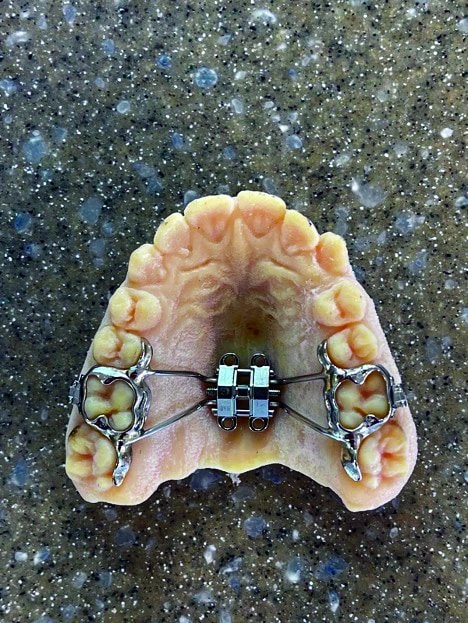
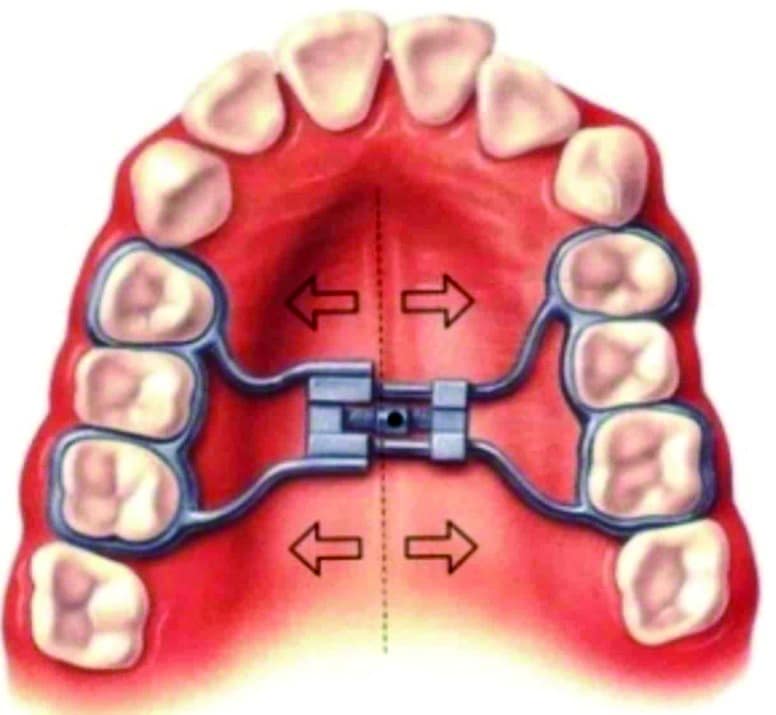
Skeletal transverse expansion involves increasing the transverse dimension of the maxillary/mandibular basal bone, providing subsequent dentoalveolar expansion as well. The maxilla is the most commonly expanded facial bone, and achieving true skeletal expansion of the maxilla also increases the dimensions of the nasal cavity, subsequently reducing nasal breathing constriction. For children with primary and mixed dentition, maxillary skeletal expansion can be achieved by any number of Rapid Palatal Expansion (RPE) devices including banded or bonded Haas or Hyrax design (Figure 7). In the permanent dentition, maxillary skeletal expansion can still be achieved; however, a significant amount of dental tipping of the molars can also occur. For this reason, our office has chosen to utilize Micro-implant Assisted Rapid Palatal Expanders (MARPE) for all permanent dentition cases (Figure 8). In multiple studies, MARPE appliances have been shown to achieve superior skeletal expansion and less dental tipping in the permanent dentition.1
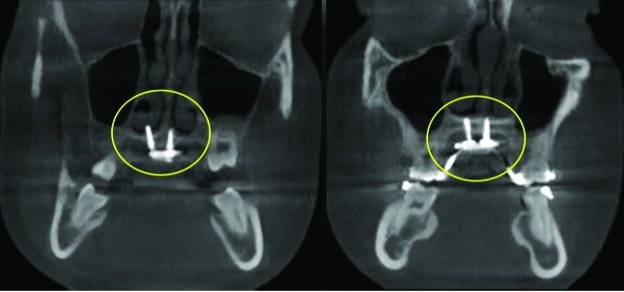
Historically, Surgically Assisted Rapid Palatal Expansion (SARPE) was the only predictable strategy to achieve true skeletal maxillary expansion in adults. This procedure essentially involved performing LeFort I osteotomies, without doing a maxillary downfracture, to reduce the resistance to skeletal expansion. A tooth-borne RPE was then fabricated and installed, and an expansion screw was activated daily to achieve skeletal expansion with predictable results (Figure 9). With cone beam computed tomography (CBCT) radiographs and custom 3D metal printing more prevalent, a custom-fabricated MARPE can now achieve predictable non-surgical expansion in adults of any age (Figure 10).
MARPE technique
The technique for delivering a MARPE has been improving since our office first started placing them in 2019, and our current technique adheres to the following guidelines
- Chlorhexidine gluconate (.12%) rinse for 60 seconds.
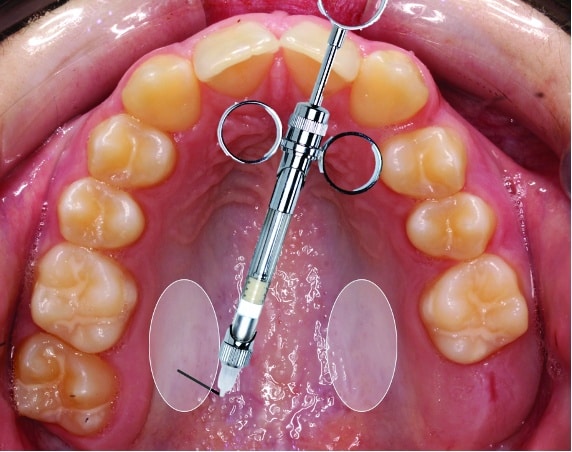
- Apply topical anesthesia (20% Lidocaine, 4% Tetracaine, 2% Phenylephrine) over the greater palatine foramen for 5 minutes, wipe, then wait an additional 5 minutes (Figure 11).
- Administer ¼-½ carpule of 4% Citanest Forte with a 30-gauge syringe bent at a 90-degree angle (Figure 12).
- Cement the appliance with 3M Multi-Cure Glass Ionomer Orthodontic Band Cement.
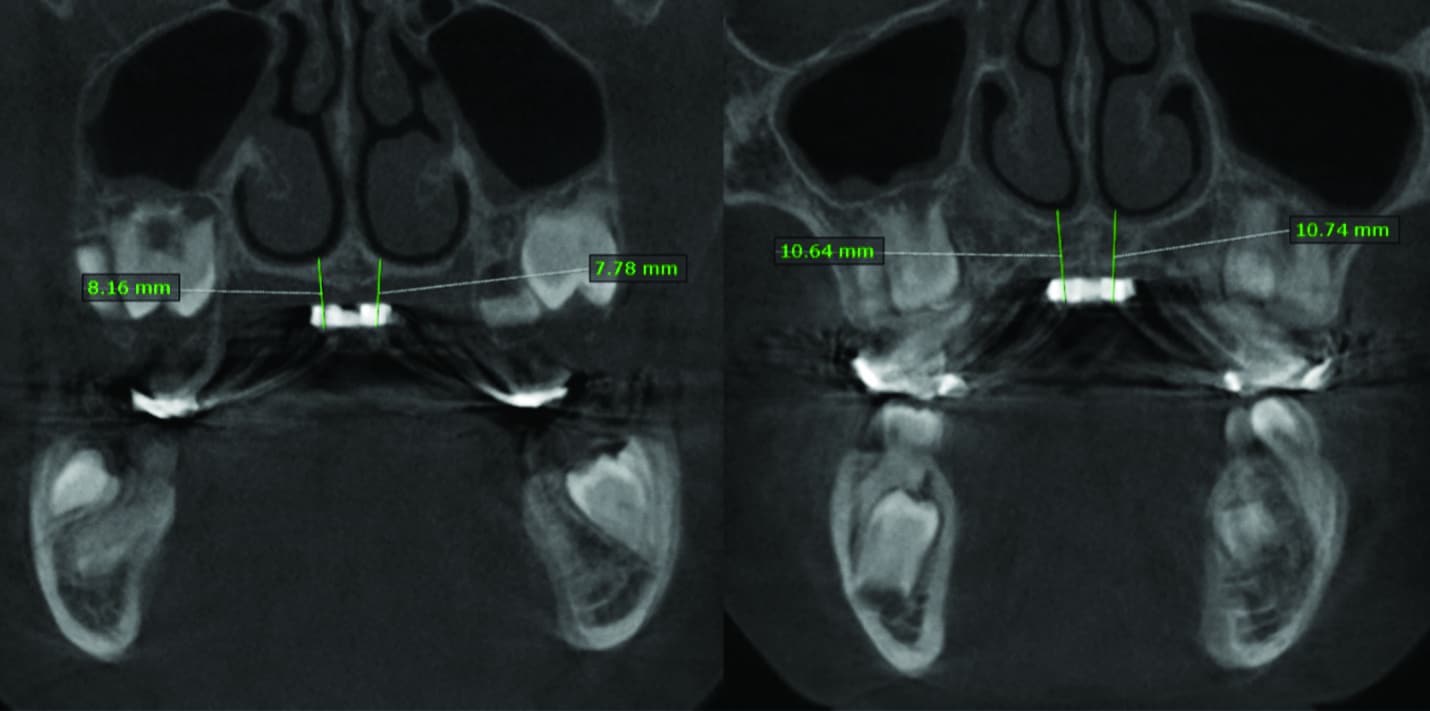
- Take the first CBCT to measure for appropriate TAD lengths (Figure 13).
- After ensuring that the palate is completely numb, insert the TADs using an electric TAD driver.
- Take the second CBCT to ensure bicortical engagement of the TADs (Figure 14).
Note that these guidelines serve as suggestions and do not substitute for taking a comprehensive course in MARPE/TAD placement.
There has been much discussion about the best rate of activation of maxillary expanders, and there are several schools of thought. Current thinking is that slow expansion (1 turn/day) provides the most predictable expansion while giving trans-septal fibers adequate time to respond. This helps to prevent patients from experiencing large diastemata, which can rip trans-septal fibers and cause loss of interdental papillae. OP
All case images courtesy of Robert “Tito” Norris, DDS.
Reference

Robert “Tito” Norris, DDS, is a board-certified orthodontist in private practice at Stone Oak Orthodontics in San Antonio, Tex. A graduate of the University of Texas Health Science Center at San Antonio Dental School, he completed a general practice residency at the VA hospital in Washington, DC, and his orthodontic specialty training at Howard University. After serving as a U.S. Air Force orthodontist, he returned to San Antonio to open his practice. Norris, who lectures both nationally and internationally, holds several patents and trademarks, and is the inventor of the Norris 20/26 Passive Self-Ligating Bracket System.