by Dipak Chudasama, BDS, MSC, MOrth RCS; and Laurance Jerrold, DDS, JD
A new product designed to maximiize both stability and looks
 |
| A new product designed to maximize both stability and looks |
It has been said that the aim of orthodontic therapy is to promote health, restore function, and create beautiful smiles. These goals are usually attained by initiating tooth and/or skeletal changes that lead to the desired result. Achieving these results, however, is rather easy compared to maintaining them. Much to the dismay of all orthodontists, finishing occlusal relationships to perfection does not ensure postretention stability.1 Little noted that, without lifetime retention, the strategy of arch development will yield unacceptable results.2 One fact of life that is consistently predictable is that mandibular arch length and width continue to decrease over time.3,4
The causes of incisor irregularity following orthodontic movement have been investigated for many years. A review of the literature with regard to incisor relapse and irregularity suggests that this is a multifactorial manifestation. The integrity of the supporting periodontal and gingival tissues, the influence of environmental factors and neuromuscular influence, continued growth, pretreatment occlusal relationships, thinner bone support in the mandibular cortex,5 latent mandibular growth, and developing third molars are just a few of the factors related to postretention crowding. It has been hypothesized that changes in arch form and shape6 and increased incisor proclination, when coupled with the anterior component of force,7 are other reasons for increased incisor irregularity following orthodontic treatment. Although numerous factors have been reported to play a role in post-treatment crowding, no definite conclusions regarding the relative contribution of these factors can be reached.8
 |
| Dipak Chudasama, BDS, MSC, MOrth RCS |
 |
| Laurance Jerrold, DDS, JD |
Retention should be customized to the patient and include such parameters as occlusion, aesthetics, growth, and function. Retention should also be related to the treatment plan chosen, the mechanotherapy employed, the results achieved, and the potential for the patient to cooperate with the retention protocol. While there is no universally recognized or accepted time period for retention, Littlewood noted that it takes, on average, a minimum of 232 days for the fibers around the teeth to remodel to the new tooth position.9 Reorganization of the periodontal ligament occurs over a 3- to 4-month time period, while the supracrestal fibers of the gingiva take up to 12 months to reorganize.10 However, with constriction of the arch length and arch width continuing well past the cessation of growth, retention should not be abandoned after conforming to the time parameters for reorganization of the periodontal structures.11
With these facts as our baseline, it is easy to see that retaining postorthodontic alignment becomes a real clinical challenge. The orthodontist should not assume that stability will occur, but should assume instability will likely be the pattern. Once that posture is adopted, the practitioner can plan against and prevent (or at least minimize) undesirable change.12
Methods of Retention
Since the realization that the alignment of dental units achieved as a result of orthodontic tooth movement is not likely to remain relatively stable without assistance, various methods of retention have been explored. These have included—but are not limited to—a cuspid-to-cuspid banded lingual bar, acrylic retainers of various design, clear-plastic (Essix)-type retainers, and fixed lingual wire retainers.13–15
Aasen and Espeland advocate a protocol that they believe eliminates the use of any type of retention appliance through overcorrection of rotations and interproximal enamel reduction.16 To ensure alignment in the apical area, the technique involves placing a heavy rectangular archwire at the end of treatment for at least 2 to 3 months. As an alternative to issuing a mandibular retainer, this method calls for additional interproximal reduction to resolve crowding during retention follow-up.
 |
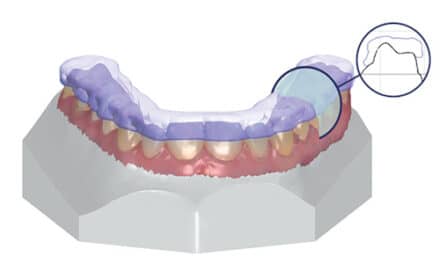
| Figure 1: A BioMers ASTICS retainer. |
 |
| Figure 2: A BioMers ASTICS retainer with a pink wire. |
With the understanding of inherent instability, many orthodontists have used bonded retention to help maintain alignment and withstand the expected decreases in arch width and length.
Aesthetic Retainer Options
There are several drawbacks to conventional retainer designs, and the profession accepts that there are limitations to what we currently have. From the patient’s perspective, aesthetic options appear to be few and limited. Contemporary materials have been developed that offer strength, flexibility, pleasing aesthetics, and biocompatibility. Fiber-reinforced composites (FRCs) have been developed as aesthetic and metal-free alternatives for various dental materials, including prosthodontic bridges and crowns, periodontal splints, and orthodontic retainers.19–21
Recently, the BioMers ASTICS™ retainer was introduced for testing at the School of Orthodontics at Jacksonville University. A total of 21 patients are undergoing a pilot study with the appliance. The appliance consists of a translucent BioMers ASTICS wire in the anterior section, which is embedded into a hollow metal tube in the posterior portion of the framework. This assembly is available in different designs, including Hawley, Wrap-around, and Spring. Using Little’s irregularity index22 as the criteria, measurements that were collected at monthly follow-up visits showed that these retainers maintain orthodontic correction excellently.
The advantage of the BioMers ASTICS labial bow is that not only does it come in clear wire for those desiring a less visible wire, but it also can be manufactured in a variety of colors for those who wish to spice up their retainer visibility. The underlying design also makes the labial bow resistant to staining, material fatigue, and monomer sensitivity. Figures 1 to 4 show the new BioMers ASTICS retainer. Figure 2 depicts the retainer with a pink wire, one of four colors to be released later in 2008. This appliance offers the profession what it has been long seeking: aesthetic control over arch length and width stability in the post treatment environment.
 |
| Figure 3 and 4: A BioMers ASTICS retainer in the mouth. |
Dipak Chudasama, BDS, MSC, MOrth RCS, is an associate professor at Jacksonville University School of Orthodontics, Jacksonville, Fla. He can be reached at
Laurance Jerrold, DDS, JD, is the dean and program director of postgraduate orthodontics at Jacksonville University School of Orthodontics and is a nationally recognized dental risk-management educator. He can be reached at
References
- Ormiston JP, Huang GJ, Little RM, Decker JD, Seuk GD. Retrospective analysis of long-term stable and unstable orthodontic treatment outcomes. Am J Orthod Dentofacial Orthop. 2005;128:568-574.
- Little RM. Stability and relapse: Early treatment of arch length deficiency. Am J Orthod Dentofacial Orthop. 2002;121:578-581.
- Little RM, Riedel RA. Årtun J. An evaluation of changes in mandibular anterior alignment from 10-20 years post-retention. Am J Orthod. 1988;93:423-428.
- Bramante MA. Controversies in orthodontics. Dental Clinics of North America. 1990;34:91-102.
- Rothe LE, Bollen AM, Little RM, Herring SW, Chaison JB, Chen CSK, Hollender LG. Trabecular and cortical bone as risk factors for orthodontic relapse. Am J Orthod. 2006;130:476-484.
- De La Cruz A, Sampson P, Little RM, Årtun J, Shapiro PA. Long-term changes in arch form after orthodontic treatment and retention. Am J Orthod Dentofacial Orthop. 1995;107:518-530.
- Acar A, Alcan T, Erverdi N. Evaluation of the relationship between the anterior component of occlusal force and postretention crowding Am J Orthod Dentofacial Orthop. 2002;122:366-370.
- Blake M, Bibby K. Retention and stability: a review of the literature. Am J Orthod Dentofacial Orthop. 1998;114:299-306.
- Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Orthodontic retention: A systematic review. J Orthod. 2006;206:205-212.
- Joondeph DR. Retention and Relapse. In: TM Graber, Ed. Orthodontics: Current Principles and Techniques. St Louis: Elsevier; 2005:1123-1151.
- Little RM, Riedel RA, Stein A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97:393-404.
- Little RM. Stability and relapse of dental arch alignment. Br J Orthod. 1990;17:235-24.
- Angle EA. Treatment of malocclusion of the teeth. 7th ed. Philadelphia: SS White Manufacturing Co, 1907.
- Hawley CA. A removable retainer. Int J Orthod. 1919;2:291-298.
- Lindauer SJ, Shoff RC. Comparison of Essix and Hawley retainers. J Clin Orthod Dentofacial Orthop. 1998;32(2):95-98.
- Aasen TO, Espeland L. An approach to maintain orthodontic alignment of lower incisors without the use of retainers. European J Orthod. 2005;27:209-214.
- Knierim RW. Invisible lower cuspid to cuspid retainer. Angle Orthod. 1973;43:218-219.
- Bearn DR. Bonded orthodontic retainers: a review. Am J Orthod Dentofacial Orthop. 1995;108:207-213.
- Geserick M, Ball J, Wichelhaus A. Bonding fiber-reinforced lingual retainers with color-reactivating flowable composites. J Clin Orthod. 2004;38:557-559.
- Burstone CJ, Kuhlberg AJ. Fiber-reinforced composites in orthodontics. J Clin Orthod. 2000;34:271-279.
- Freudenthaler JW, Tischler GK, Burstone CJ. Bond strength of fiber-reinforced composite bars for orthodontic attachment. Am J Orthod Dentofacial Orthop. 2001;120:648-653.
- Little R. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod Dentofacial Orthop. 1975;68:554-563.