Phillip M. Goodman, DDS, MSc, PhD
Dayton, Ohio

Goodman
Talk about early: It has been theorized that around 400 to 500 BC, Hippocrates and Aristotle contemplated ways to straighten teeth. Ancient mummies have been discovered with metal bands around their teeth and cat gut strung between them to provide the force used to move the teeth and close spaces.
A French dentist, Pierre Savagn, took dentistry out of the Dark Ages. He published a book called The Surgeon Dentist in 1728, which included methods for straightening teeth. Savagn used an appliance called the “Blandeau,” which was an iron horseshoe-shaped device used to help expand the arch. He recommended that the patient eat a lot of grapes while the appliance was being worn because he thought, erroneously, that the acid in the grapes would prevent the appliance from rusting in the mouth.
We have certainly come a long way in our profession since then. However, some of the basic principles, if not the appliances, remain similar.
The following is my philosophy on early orthodontic treatment: We can do our patients a great service with early intervention in certain types of developing malocclusions. We must also understand, however, that not all patients that come to us in mixed dentition need our services. It is up to us as clinicians and good diagnosticians to make that distinction.
Here’s what I look for when a new patient arrives in my consultation room:
- How does the young patient feel about his appearance? If he is old enough to evaluate himself in the mirror, it will give the clinician good insight as to the avenue of treatment to follow. Remember that patients’ perception of themselves is more important then our perception of patients.
- Is there is a skeletal issue present? If so, can we correct it with functional orthopedics? Here we see crossbites, open bites, Class II malocclusions with protrusions, developing Class III malocclusions, etc.
- From there we look at musculature. Are there thin vermillion borders, tight orbicularis and masseteric musculature, tongue habits (either thrusting or reverse swallowing)? This could mean that some of our functional orthopedics may be nullified. So we must overcorrect in these instances or hold longer in the retention phase of our first-phase treatment.
- Are the teeth in harm’s way? If so, we must begin treatment to retract the maxillary anterior teeth so they can avoid injury.
- Is there a psychological implication? As we know, kids can be cruel to other kids, especially if they find a sensitive area that can be picked on. For example, a young lady came to see us who had very square teeth, blond hair, freckles, and diastemata between all the anterior teeth. She was taunted with the name “Sponge Bob” so much that she did not want to go to school. Once we closed the diastemas, the name-calling ceased and she was once again happy.
- If a patient comes in with severe crowding, we will use holding arches along with selective deciduous extraction until we can do a full treatment.
- The last intervention we will do is to correct an occluded airway by suggesting tonsillectomy and/or adenoidectomy. The patient is then placed on regular recall so we can watch her development. Many times Mother Nature will do a wonderful job in helping to correct the malocclusion once the airway has been restored.

If it can possibly be avoided, we try not to place brackets in a Phase I treatment. There are a myriad of reasons for this, most of which I am sure you have already faced.
Orthodontists certainly have the armamentarium to help many young patients on their way with a beautiful smile, which in turn will help to build their self-esteem early in life.
We, as practitioners, can’t ask for more than that.

Astuto
Laser Pointers
Steven Astuto, DDS, MSD
Amarillo, Tex
I have been using a soft-tissue laser for about 1 year now. I was hesitant at first, since I didn’t want to use anesthesia and possibly scare my young patients, but now I use it almost every day in my practice.
I use a compounding gel made locally for 5 minutes on the gums to be lasered prior to the procedure. This usually gives good anesthesia. I also use a ceramic bur prior to using the laser. This bur is amazing. I don’t know how it works, but it is fast and allows for good sculpting of the tissue. Then I use the laser for homeostasis and final sculpting of the soft tissue.
I had a hard time charging for this procedure initially, but now I charge per tooth that has had a gingivectomy. I got the insurance codes and filed for these procedures.

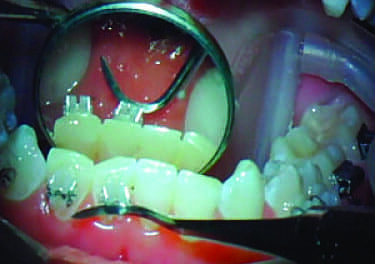
Left to right: a patient pregingivectomy, immediately postgingivectomy, and 2 weeks after gingivectomy.

Petrey
Mechanics for Anterior Open-Bite Correction with TADs
Joseph S. Petrey, MPH, DMD, MS
Somerset, Corbin, and Hazard, Ky
Anterior open bites are one of the more challenging malocclusions for clinicians to treat. An effective treatment modality is to use TADs placed to the buccal with powerchain or Nikodem® springs placed from the TAD, wrapped under the wire and back to the TAD to intrude the posterior segments. The problem with this technique is that the force is placed at a distance from the center of resistance to the teeth, and can cause a buccal rotation that can lead to plunging lingual cusps, potentially exacerbating the open bite.

An eyelet bracket bonded to the first molar and attached to a TAD with powerchain.
To combat this, a Transpalatal Arch (TPA) can be attached to resist this rotation. While mechanically sound, the TPA can lead to more patient discomfort and can slow intrusion because the entire unit must intrude together. TPAs also require added laboratory time and cost, and can have a considerable negative effect on speech and hygiene.

Two palatal TADs can intrude the posterior segments.
An alternative method for posterior intrusion with TADs, which controls rotation without the use of TPAs, is to place additional palatal TADs and use eyelet brackets on the first molar’s lingual surface. Two TADs can be placed in the palate between the second premolar and first Molar. (I recommend placing them with a contra-angle ratchet or hand driver.) As there is no wire to attach to on the lingual, you can bond an eyelet bracket (I use the Traction Hook from TP Orthodontics) to the lingual surface of the first molar and attach powerchain from the TAD, through the eyelet, and back to the TAD. With equivalent powerchain placed buccally and palatally, you can achieve controlled intrusion without using a TPA. This setup also allows for easy activation, with simple looping of powerchain at each visit and greater comfort for the patient.
This same setup can also be used for single-tooth intrusion, segmental intrusion, or with no wires at all if angulation and direction of force is accounted for.