By Shawn L. Miller, DMD, MMedSc

We recommend PAOO for almost any patient willing to accelerate their time in braces. Certainly with the ever-increasing pace of modern society, offering 6 to 9 months of treatment duration versus 18 to 24 months is a tremendous advantage. However, beyond treating traditional orthodontic cases quicker, we found that with PAOO we could blur the line between orthognathic surgical care and traditional standard care. For many discrepancies, including Class III malocclusions, open bites, narrow arches, and some Class II malocclusions, we are able to successfully avoid orthognathic surgery while still achieving desired esthetic and functional goals.
Unfortunately, in today’s health care landscape, it has become increasingly difficult to provide treatment involving orthodontics in combination with orthognathic surgery. There are unique challenges accompanying orthognathic surgical care, all of which require more time, energy, and expense for both the doctors and patient. With increasing health care costs, especially associated hospital expenses, paying for orthognathic surgery without adequate health insurance is not feasible for many families and patients. Even if a patient has adequate medical insurance, compounding the problem is the difficulty of getting orthognathic surgical procedures approved by insurance carriers and having them deemed medically necessary. If a patient is fortunate enough to get insurance approval, in many geographic areas finding an oral and maxillofacial surgeon willing to participate with a particular insurance plan can be nearly impossible. With insurance reimbursement not keeping up with inflation and medical expenditures, many oral surgeons refuse to participate with many insurance plans, or simply may have just stopped providing orthognathic surgery.
Treatment
The surgical protocol and description of the PAOO procedure is presented elsewhere,1-3 and the biological foundation is well-reported in the literature.4-8 The PAOO is performed under intravenous sedation by trained periodontists or oral surgeons, and involves corticotomies to accelerate tooth movement and bone grafting (demineralized freeze-dried bone allografts and Bio-Oss®) to enhance bone volume after remineralization. The corticotomies can be done in localized areas of interest, or generalized to entire arches, as prescribed by the orthodontist. After sutures are placed, the patient is given prescriptions for antibiotics, Chlorohexidine rinse, and non-anti-inflammatory analgesics. Following the procedure, the patient is seen every 2 weeks for orthodontic adjustments. Treatment progress is accelerated and condensed, so frequent wire changes are necessary, elastics are given much earlier, and finishing procedures are instituted much sooner. There is approximately a 6- to 9-month window of opportunity before remineralization occurs, in which the accelerated movement subsides. Morbidity and mortality are theoretically significantly less with PAOO, particularly because general anesthesia is not necessary and a hospital stay (potential nosocomial infections) is not required.
The following are two cases, both Class III malocclusions, where we utilized PAOO to avoid orthognathic surgery.
Case 1: Eric

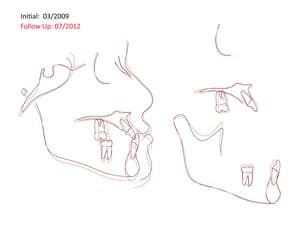
Our diagnostic workup showed that some key issues for Eric were his dental and skeletal Class III relationships, negative overjet, posterior crossbite, mild crowding, and general misalignment (Figure 1 and Figure 2A). Some other concerns were a moderate cant (higher on left), midline discrepancy, and deep Curve of Spee. Periodontally, Eric had good oral hygiene, but had some areas with thin gingival attachment and a few areas in the beginning stages of recession. On the CT scan, thin alveolar buccal bone was noted, which is a very common finding.

The occlusion and esthetics were outstanding at 9 months. However, Eric was very particular about minor cosmetic discrepancies, so an additional 2 months were spent with some very precise finishing movements. Total treatment time was therefore 11 months. A mandibular fixed retainer bonded canine to canine was given (it has since been changed to a clear vacuformed retainer), and a maxillary vacuformed retainer were given. The retainers were instructed to be worn full-time for 1 week followed by night-only wear indefinitely. Final photographs were taken at the conclusion of treatment (Figure 2B), and the follow-up records were taken 2 years after braces removal (Figure 2C and Figure 3).
Case 2: Mike
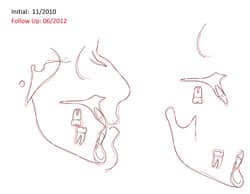
Mike presented to our office as a 21-year-old young adult seeking to improve both his occlusal function and esthetics, in particular his open bite. After our standard orthodontic examination and consultation, we took thorough orthodontic records, including a cone beam CT scan, mounted models, and photographs.

Our goal was to correct his Class III dental relationship and develop proper anterior guidance systems with appropriate overjet and overbite. Esthetically, we felt it was equally important to enhance his smile by broadening the upper arch, improving lip support, and providing more tooth display upon smiling. We did not want to camouflage by retracting lower anteriors via temporary anchorage devices, IPR, and/or extractions. Minimizing the length of time in treatment was also an important consideration for Mike. Therefore, we developed a plan centered on PAOO for the maxillary arch, with the caveat that if we were unsuccessful attaining our goals, orthognathic surgery would be utilized for final correction.


Conclusion
References
1. Ferguson DJ, Wilcko WM, Wilcko MT. 2006. Selective alveolar decortication for rapid surgical-orthodontic resolution of skeletal malocclusion. In: Bell WE and Guerrero C, eds. Distraction Osteogenesis of the Facial Skeleton. Hamilton, Ontario, Canada: BC Decker.
2. Wilcko WM, Ferguson DJ, Bouquot JE, Wilcko MT. Rapid orthodontic decrowding with alveolar augmentation: case report. World J Orthod. 2003;4:197-205.
3. Wilcko MT, Wilcko WM, Bissada NF. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Seminars in Orthodontics. 2008;21(4):305-316.
4. Frost HA. The regional acceleratory phenomena: a review. Henry Ford Hosp Med J. 1983;31:3-9.
5. Gantes B, Rathburn E, Anholm M. Effects on the periodontium following corticotomy-facilitated orthodontics. J Periodontol. 1990;61:234-238.
6. Twaddle BA, Ferguson DJ, Wilcko WM, Wilcko MT, Lin CY. Dento-alveolar bone density changes following accelerated orthodontics. J Dental Res. 2002;80:301.
7. Yaffe A, Fine N, Bindermen I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J Periodontol. 1994;65:79-83.
8. Lino S, Sakoda S, Ito G, Nishimori T, Ikeda T, Ikyawaki S. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am J Orthod Dentofacial Orthop. 2007;131:448.e l-8.
 |
Shawn L. Miller, DMD, MMedSc, is in private practice in Orange and Aliso Viejo, Calif. He completed his dental degree at the University of Pennsylvania and his Masters of Medical Sciences and orthodontic residency at Harvard University. He lectures locally on PAOO, Incognito, and Interdisciplinary Orthodontic Treatment. He is Board Certified by the American Board of Orthodontics. He can be reached at [email protected]. |








