by Alfredo Gilbert, DDS, MS
Predicting cooperation can improve your clinical results
 |
Several researchers and dental practitioners have studied the possibility of anticipating certain behavioral traits, such as cooperation, in order to improve success during treatment.1,2 In orthodontics, where the relationship between the orthodontist and patient extends over a long period of time (years, perhaps), it is particularly useful to predict cooperation during treatment. This becomes more relevant when considering the influence cooperation or noncooperation can have on issues like appointment attendance, care of appliances, and hygiene
Surprisingly, a quick review of the literature concerned with predicting cooperation/compliance shows a multiplicity of (often contradictory) results. While some have found statistically significant relations between cooperation and internal (personality) or external (social) factors, others have found none, suggesting the relationship is dependent on other factors as well.
Although hundreds of articles have been dedicated to this issue, none has yet explored cooperation in lingual orthodontic patients. In order to assess lingual patients’ cooperation, I used two questionnaires: the well-known Orthodontic Patient Cooperation Scale (OPCS),3 designed to be filled by the specialist, and Goldberg’s International Personality Item Pool (IPIP).4
The main purpose of this study is to evaluate whether or not there is a relationship between certain personality traits and the degree of cooperation of the lingual patient during treatment. Furthermore, this study foresees the possibility of anticipating a lingual patient’s cooperative behavior by including certain personality-related questions in the clinical history.
Why Cooperation?
As stated before, the treatment’s outcome is strongly influenced by the patient’s cooperation. Clinical experience shows how patients unwilling to cooperate (by causing continuous appliance breakages, for example) tend to extend the length of treatment and compromise its quality. In extreme cases, a patient’s noncompliance with the orthodontist’s instructions can lead to tense situations and, eventually, a halt of treatment.
In my experience, it is not unusual to receive patients who have previously started orthodontic treatment and stopped, only to discover that the underlying reason was not the previous orthodontist’s incompetence but the patient’s unwillingness to cooperate.
When patients with these characteristics come for treatment, orthodontists find themselves at a moral crossroads: Should you begin or continue a treatment with low possibilities of success or deny treatment altogether?
Clearly, our medical ethics impede us from denying treatment to a person whose life quality will be improved as a consequence of treatment. Yet, many orthodontists would benefit clinically and interpersonally if noncooperative patients could be identified before starting treatment. Needless to say, patients with noncooperative traits will most likely continue that way. However, a better-oriented strategy might lead to greater success in treatment.
Why Personality?
Clinical experience has showed that noncooperative patients tend to frustrate orthodontic efforts to a greater extent than cooperative ones. In a way, many orthodontic practitioners intuitively know that certain types of personalities are more likely to hinder treatment than others. Yet, most of us are unlikely to follow our intuition. Besides, few of us can fully grasp the slippery concept of “personality.” What do we mean by it? How are we to understand and put into scientific terms what theologians consider to be man’s essence and soul?
As difficult as it may seem, several researchers have dealt with this issue. Theodore Millon, for example, has created a whole biosocial system for dealing with personality.5 In his study, personality is understood as a biopsychosocial continuum, which can be divided into five dimensions: behavioral appearance, interpersonal conduct, cognitive style, affective expression, and self-perception.
Furthermore, Millon recognizes four characteristics present in what he considers to be a “healthy personality”: autonomy, adaptability, emotional stability, and self-actualization.
Perhaps the most widely accepted personality model is the Five Factor Model (FFM), introduced in 1933 by L.L. Thurstone. The five factors are the following: openness, conscientiousness, extraversion, agreeableness, and neuroticism. Each of these contains a series of more specific traits, although there is disagreement regarding which traits should be included under each of the factors.
 |
| Alfredo Gilbert, DDS, MS |
Nonetheless, the question remains: Is there a certain type of personality more likely to be noncooperative? If so, is there a way to determine a priori the existence of such personality traits?
If such a possibility exists, then we must rely on an instrument to convert subjective intuition into objective prediction. Therefore, it is indispensable to borrow from psychological research in order to find those personality traits that may predict cooperation. Unfortunately, no straightforward test exists for recognizing a cooperative personality. Yet organizational physiology has dealt widely with the issue, with the intention of improving teamwork among group members.6
Drawing on psychological research, we may say that people are situated somewhere along a continuum of absolute cooperativeness on one side and absolute individualism on the other.7 Therefore, it would be almost impossible to say that people are either cooperative or individualistic; rather, each person is closer to one of these two poles. Keeping this is mind will help avoid a common mistake: Researchers tend to look for correlations between certain variables (age, gender, socioeconomic situation, personality) and cooperation, rather than correlations between extreme cases and cooperation.
A study has suggested this idea already.8 Applying two special psychological tests (the Dental Sentence Completion Test and the Dental Thematic Apperception Test), the researchers tried to predict compliance among psychotic patients. Among their observations was that, although the correlation between predicted and actual behavior was not high enough, extremes do seem to be able to predict behavior.
It is for this reason that my study investigated the correlation not simply between personality and cooperation but between cooperation and highly noncooperative personality traits.
Why Lingual Orthodontics?
My clinical experience strongly demonstrates a greater need for compliance during lingual rather than labial treatment. The reason is simple: Labial orthodontics, at worst, present discomfort on the labial surface and transient pain. Only a very small percentage of patients will take conscious action to remove previously set appliances.
However, as aesthetically (and sometimes clinically)9 convenient as they may be, lingual orthodontics appliances do obstruct the patient’s natural bite. Naturally, for most patients this does not represent a major problem. Since we are dealing with a neuromuscular reflex, the brain rapidly (usually in less than a week) instructs the muscles to adjust to the new reality, changing the bite to a less deep one. The patient generates a temporary compensatory reflex that does not interfere with his daily routine.
Nevertheless, some patients have difficulties adapting to lingual appliances. Anxious patients, for example, tend to experience greater discomfort, associated to a large extent with a psychological state. Being set in the interior surface of teeth, lingual applies can be more easily removed by the patient’s bite, thus affecting treatment outcomes. It is for this reason that predicting patient cooperation becomes ever more relevant for lingual orthodontists.
 |
|
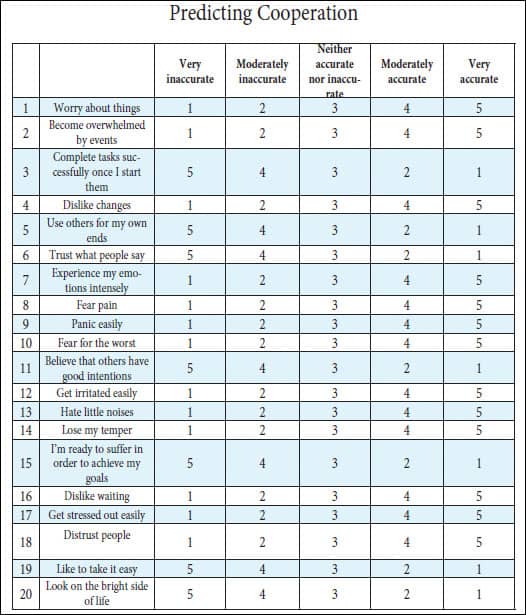
Patients were asked to use the rating scale next to each phrase to describe how accurately each statement describes them. For the purposes of the study, each answer was assigned a numerical value as shown. Scoring was as follows: 20 to 40 points: High Cooperativeness. Few problems are expected to derive from cooperation during treatment. The patient is likely to comply with most lingual orthodontic indications. 40 to 80 points: Medium Cooperativeness. No prediction can be made regarding the patient’s cooperativeness. 80 to 100 points: Low Cooperativeness. Noncompliance can be expected. Conflict may arise due to appliance breakages, missed appointments, and poor hygiene. The orthodontist may suggest labial treatment instead.
|
Methodology
Two questionnaires (the OPCS and the IPIP) were given to a sample of 42 adults (25 women and 17 men), ranging from 21 to 40 years old, who were undergoing lingual orthodontic treatment at the ClÍnica Dental Metropolitana in Mexico City. All of them had been in treatment for at least 3 months.
The OPCS10 is a 10-question form that evaluates a patient’s cooperation, according to the orthodontist’s perception. Each of these questions is formulated in a five-point format, ranging from “always” to “never.” Each answer was given a numerical value, and the total was expressed in a final score, ranging from 10 (lowest cooperation) to 40 (highest cooperation).
Among the statements included in the OPCS are the following:
- “This patient complains about treatment procedures;”
- “This patient demonstrates excellent oral hygiene;” and
- “This patient’s behavior is sullen, hostile, belligerent, or rude.”
Several instruments have been developed for measuring the five FFM. One of the most comprehensive, developed by American psychologist Lewis R. Goldberg, PhD, consists of 1699 items. Based on this, several representative models have been developed, such as the NEO PI-R, authored by Paul T. Costa, Jr, and Robert R. McCrae. In my study, the Short Form for the IPIP-NEO, consisting of 120 items, was given to each of the 42 patients.
I used the X2 test with Yates correction to find a significant (P ? .05) association between cooperation and personality. Following the idea that only extreme cases can show a positive correlation, only those patients scoring less than 15/40 points on the OPCS were considered “noncooperative.” Similarly, only those scoring “high” or “low” on the IPIP-NEO (that is, the top and lowest 30%, when compared with people of the same age and gender in Mexico) were considered. “Average” cases, therefore, were left out of the evaluation.
The IPIP gives results for five domains and 30 subdomains. All subdomains were considered and submitted to the X2 test.
Results
Of the 30 subdomains, only eight were statistically significant. Interestingly, two clusters, “agreeableness” and “neuroticism,” contained 87.5% of the statistically significant subdomains, very much like Saulsman and Page predicted.11
The “extraversion” and “openness to experience” clusters showed no correlation with any of its subdomains.
In the “conscientiousness” cluster, only dutifulness was significant. Among those who were rated “low,” 60% were noncooperators.
Low levels of “agreeableness” were also determinants of noncooperativeness. Among “low”-trust patients, 57% were noncooperators. Patients scoring “low” in morality were noncooperators 66% of the time. Patients who the IPIP-NEO test said were “low” cooperators were largely noncooperating at the OPCS test (75%). Those scoring “low” in sympathy were noncooperators 66% of the time.
The relationship between “neuroticism” and cooperation was inverse: Highly neurotic patients were mostly noncooperators. The strongest relation was found regarding anxious patients: 77% of patients with “high” levels of anxiety were noncooperators. Patients with “high” anger were noncooperators 60% of the time. Those scoring “high” in depression were noncooperators 71% of the time.
Not surprisingly, when taken as whole clusters, only agreeableness and neuroticism proved to be significant. Highly agreeable patients (those in the highest 30%) were cooperative 83% of the time, while disagreeable patients (those in the lowest 30%) were noncooperative 62% of the time. Regarding “neuroticism,” 81% of less neurotic patients were cooperative, while 64% of highly neurotic patients were noncooperative.
Toward a Personality-Oriented Clinical History
These results can only point toward the necessity of including personality-related questions in orthodontic clinical histories. However, a very real tension remains: How to make a questionnaire short enough to be included as part of the clinical history while still maintaining statistical veracity? Is there a way to predict patient cooperation through a shorter, Likert-type instrument?
Obviously, 120 questions are unviable for the average new orthodontic patient. However, as proved by the results, statistical significance was found mainly in two of the five clusters. A personality-oriented clinical history could be designed to identify only low levels of agreeableness and high levels of neuroticism. At present, I am conducting a study to evaluate a recently designed 20-item questionnaire based on IPIP questions (See the chart on page 20). Its relevance will be assessed in a forthcoming article.
Conclusion: Playing the Prisoner’s Dilemma
Game theory, a branch of applied mathematics, uses the model of the “prisoner’s dilemma” as a metaphor for portraying a situation in which two parties could gain important benefits from cooperating or suffer from the failure to do so, but end up defecting as a consequence of the high cost of cooperation. The dilemma is as follows: Two suspects are arrested and put in different cells. The police offer each one of them a deal: Testify against the other suspect and go free. If only one prisoner testifies, he goes free, but the other prisoner will get the death penalty. However, if both suspects testify against each other, each will get 10 years in prison. If nobody confesses, both will get a 1-year sentence and then go free.
Game theory explains that, since both prisoners (no matter what the other one does) will be better off by defecting, the rational choice for each to make will necessarily be noncooperation, leading them to a suboptimal solution (that is, a 10-year sentence).
However, if the dilemma were “played” repeatedly, giving each prisoner the opportunity to penalize noncooperative behavior, then both prisoners would tend to cooperate in order to achieve the best possible solution given the circumstances.
That is, when the game is played once, the rational choice is to defect. When it is played several times, the rational choice is to cooperate.
Fortunately for the orthodontist, his relationship with the patient is one of repeated games. Patients cooperate not just because of their ethical convictions but because they will face their orthodontist at their next appointment. This underscores the importance of creating a well-designed system of rewards for cooperative patients.
However, what happens when reality does not fit smoothly with theory? When patients deny cooperation, disregarding rational behavior as predicted by mathematical models?
In my clinical experience, it is evident how cooperation is a factor whose importance becomes much greater when dealing with lingual orthodontics patients for the reasons already mentioned. There may be some cases when, considering certain personality traits, the lingual orthodontist should recommend the patent a labial treatment, especially when low cooperation is expected. I guarantee this will lead to better results in treatment.
Alfredo Gilbert, DDS, MS, is a guest professor of lingual orthodontics at the Hospital Infantil du Mexico Federico Gomez and the academic coordinator of lingual orthodontics at the Facultad de Estudios Superiores of the Universidad Nacional AutÓnoma de MÉxico. He is the author of Lingual Orthodontics: The Truly Invisible Orthodontics, and teaches a hands-on lingual course at NYU. He can be reached at
References
- Mandall NA, Matthew S, Fox D, Wright J, Conboy FM, O’Brien KD. Prediction of compliance and completion of orthodontic treatment: are quality of life measures important? Eur J Orthod. 2008;30(1):40-45.
- Nanda RS, Kierl MJ. Prediction of cooperation in orthodontic treatment. Am J Orthod Dentofacial Orthop. 1992;102(1):15-21.
- Slakter MJ, Albino JE, Green LJ, Lewis EA. Reliability and stability of the Orthodontic Patient Cooperation Scale. Am J Orthod. 1980;60:253-289.
- International personality item pool. Available at: ipip.ori.org. Accessed June 24, 2009.
- Theodore M, Everly GS. Personality and Its Disorders: A Biosocial Learning Approach. New York: John Wiley and Sons; 1985.
- Chatman JA, Barsade SG. Personality, organizational culture, and cooperation: evidence from a business simulation. Administrative Science Quarterly. September 1995.
- Liebrand WBG, McClintock CG. The ring measure of social values: A computerized procedure for assessing individual differences in information processing and social value orientation. Eur J Personality. 1988;2:217-230.
- Crowley RE. Relationship between personality factors and cooperation in dental treatment. J Dent Res. 1956;35(1):157-165.
- Gilbert A. Lingual orthodontics: the truly invisible orthodontics. Trillas, Mexico, 2008.
- Amado J, Sierra AM, Gallon A, Alvarez C, Baccetti T. Relationship between personality traits and cooperation of adolescent orthodontic patients. Angle Orthod. 2008;78(4):688-691.
- Saulsman LM, Page AC. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23:1055-1085.








