With monkeypox in the news, Orthodontic Products’ Chief Editor Alison Werner sits down with infection prevention expert Jackie Dorst, RDH, BS, for a new episode of In the Sterilization Room with Jackie to discuss the virus and how to keep the orthodontic team and patients safe.
Jackie provides a history lesson on the evolution of the monkeypox virus, which was first discovered in animals in 1958, with the first human case recorded in 1970. The current outbreak in the United States is not the first time there have been cases, or even an outbreak, in this country; however, the this current outbreak has far outpaced a 2003 outbreak where 47 confirmed and probable cases were reported across six states. As of August 2, 2002, the U.S. Centers for Disease Control and Prevention (CDC) reported 6,326 confirmed monkeypox cases in the United States. Cases have been documented in 48 states, plus the District of Columbia and Puerto Rico.
In this episode, Jackie talks about how the virus is spread and who is at risk. While the virus is primarily found in adults at this point, Jackie explains why adolescents may be at risk as more is learned about this variant of the virus. She also explains what the monkeypox rash looks like and offers these two visuals to show what the orthodontic team might encounter.

monkeypox lesion on the skin
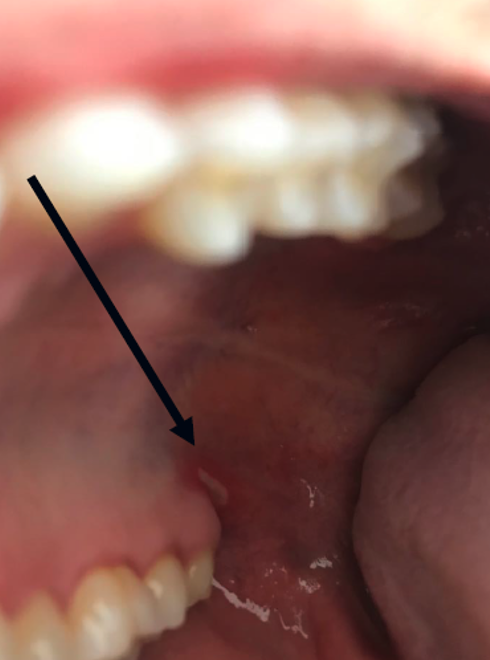
oral monkeypox lesion
Jackie then goes on to talk about treatments, vaccination, and prognosis for those who acquire the virus.
Finally, Jackie talks about why orthodontic practices should still be observing standard precautions for all patient care to mitigate the risk of monkeypox, as well as COVID, exposure, and provides a refresher on what PPE both the orthodontist and staff should be wearing when providing direct patient care. OP
Podcast Transcript
Alison Werner:
Hello, thank you for joining us for today’s Orthodontic Products Podcast on the MEDQOR Podcast Network. My name is Alison Werner, and I am the chief editor of Orthodontic Products. Today we are here with an episode of “In the Sterilization Room with Jackie,” where we talk to infection prevention expert, Jackie Dorst, about what you need to know to keep the orthodontic team and patients safe. For over 30 years, Jackie has been a consultant specializing in instrument sterilization and infection control and prevention in the dental setting. She has degrees in microbiology and dental hygiene and has been a featured speaker at the American Dental Association and the American Association of Orthodontists. Jackie, it’s so great to be with you again.
Jackie Dorst:
It’s been a while Alison, and it’s good to be back with Orthodontic Products. We know all of our orthodontic offices, we’re right in the middle of summertime now, they’re super busy with all of those summertime patients and their schedule. And then next month, they’ll be going back to school, and we’ll have a new set of challenges in front of us.
Alison Werner:
Exactly. So that’s why we wanted to have this episode to talk about something that is in the news right now, which is monkeypox. And so we wanted to do this episode to provide information to the orthodontic team about the- I guess is virus would be the correct?
Jackie Dorst:
Yes.
Alison Werner:
Okay. About the virus and about how to keep themselves safe and their patients safe during this process. So Jackie, let’s start with the basics. For those who don’t know what is monkeypox?
Jackie Dorst:
Well, I think we’ve all gotten so intimidated during the pandemic with the COVID-19, caused by the SARS-CoV-2, which was a novel, a new type of infection. Monkeypox is not. Monkeypox was first identified as an infection in mammals in 1958, and the lesions were actually identified on monkeys. However, the virus, part of the orthopoxvirus family, is transmitted in small mammals, such as maybe squirrels or rodents, or we even had an outbreak in 2003 in the United States of monkeypox in prairie dogs. So the virus is zoonotic in the animal kingdom and identified in 1958 in monkeys. And therefore was called monkeypox. It’s in the same family as smallpox.
Jackie Dorst:
The first human cases were not identified until 1970. So a decade or more later the human cases were identified, and they were usually in people who were in close contact with wild animals. At that time, we didn’t see heavy transmission, or significant transmission I guess I should say, from human to human. But as with all microorganisms and viruses, as it replicates, it can change, mutate, and we’ve learned about all those variants from the SARS-CoV-2 virus with it. So monkeypox is low transmission, and I think that’s important for the orthodontic community to know your risk of acquiring monkeypox in the ortho office is very minimal. Monkeypox requires a long skin-to-skin transmission, estimated to be almost up to a three hour exposure in a room or close proximity with somebody or exposure to the pox lesions.
Alison Werner:
Okay.
Jackie Dorst:
That they would develop on their skin. And again, this time around in the last two years, and especially with this new mutation so to speak, we’re not seeing the pox that covers the entire body as in previous decades with it. There may be only be one or two pox lesions on the hands, or the feet, or the face or maybe even inside the mouth. And unfortunately this seems to be the high risk transmission at this time is a sexual transmission for men who have sex with men.
Alison Werner:
Okay.
Jackie Dorst:
It’s been identified that in semen, there is a very high replicating viral particle count. And of course the anal type sex has more tearing and abrading of tissue, leaves those open portals for an infection to be acquired. So at this time, as the world health organization and CDC are keeping the numbers on it, it looks like 98% of the infections are in men who have sex with men or in the bisexual community. And that’s where the public health efforts are being focused right now on both vaccines and treatments with it.
Alison Werner:
Okay.
Jackie Dorst:
So back to the virus. The virus’s transmission can be respiratory, but it would mean that you’d have to be in close face to face contact with someone unmasked for three hours or more. And again, low risk with infectivity with it.
Jackie Dorst:
The second would be body fluids. And that’s what we’ve already talked about with semen. And we don’t know about saliva yet. We need more scientific research to identify are those live replicating viral particles present in saliva that increases the risk for us, and then contaminated items or what science community refers to as a fomite surface, such as a countertop, or bed linens or clothing. Can the disease be transmitted from that? And yes, if someone has active monkeypox lesions, it could be transmitted, although it’s not an efficient mode of transmission.
Jackie Dorst:
When we talked about the infectivity in previous episodes of “In the Sterilization Room” we’ve talked about the R-naught of microorganisms. If one person is infected, how many potential other people could that infect? And with measles, which is the most highly infectious, it has an R-naught of 18, meaning one infected person could potentially infect 18 other unvaccinated people with the disease. And measles can be transmitted in the air and hang suspended in the air for a long time. That’s not true of monkeypox. Monkeypox is estimated to have an R-naught of say under three with it, and you’d have to have the right mode of transmission, that close skin-to-skin contact over a period of time, where again, there’s that long exposure.
Jackie Dorst:
So there’re certain precautions. If you’re taking basic standard precautions in your office, you’re going to be at minimal to zero risk-
Alison Werner:
Yeah.
Jackie Dorst:
Of acquiring a monkeypox infection. And that’s the same for what I call your public hygiene, when we go to the grocery store, when we’re at a theater, all of the public venues that we would go into. And then also your personal hygiene. And I’m going to caution the orthodontic community because I would say over 70% of most of orthodontic patients are teenagers or middle school.
Alison Werner:
Right, yeah.
Jackie Dorst:
And they are in community activities such as sports, say wrestling, where they have a lot of skin exposed, they’re rubbing up against each other for an extended period of time. In 2008, we actually had a MRSA outbreak among wrestlers in high school communities. So wrestling teams at that time weren’t even disinfecting the mats that they wrestled on. So you can imagine with the sweat and the perspiration, if you have a MRSA lesion and it happens to rupture and that pus gets on it, that they had a number of infections. And with teenagers, maybe they have acne. And that leaves that open portal of lesion. People who have eczema or other rash type of ongoing rashes.
Alison Werner:
Okay.
Jackie Dorst:
It leaves them at risk with it.
Alison Werner:
Okay.
Jackie Dorst:
So we have this virus, low infectivity, transmitted in potentially these three ways. If you’re exposed to it, the incubation period could be anywhere from five to 21 days.
Alison Werner:
Okay.
Jackie Dorst:
Up to three weeks before you had signs of symptoms, and the symptoms are minimal with this particular mutation that we’re seeing at this time. People get well from it without any treatment.
Alison Werner:
Okay.
Jackie Dorst:
They may be sick for two to four weeks with it, and then the symptoms resolve without treatment.
Alison Werner:
Okay.
Jackie Dorst:
We do have antiviral medicines that can be used. You may hear them referred to as TPOXX is one of the antiviral medicines, and it’s Tecovirimat. And it can be administered either as pills or as an IV injection with it. So you would take it for whatever the prescribed period is, a week or maybe longer if you’re taking the oral medications. And it would reduce the symptoms for you.
Jackie Dorst:
It’s also recommended taking the vaccine if you have a high risk exposure, or even if you develop the disease that having the vaccine can reduce your symptoms with it. Now, these vaccines were the ones that were developed for smallpox. Remember? Same virus that’s in that orthopox family. And the healthcare community has treated for smallpox for over a half a century with it. You know, we know how to prevent smallpox, but smallpox vaccines were discontinued a number of years ago because it was believed that we had to eradicate it. Smallpox.
Alison Werner:
Right. Yeah.
Jackie Dorst:
But we still had a stockpile in the US and with the World Health Organization that just in case there was biological warfare, and this could be used in biological warfare, that we have those vaccines available and the antiviral treatment. So the vaccines that were created for smallpox, there is the ACAM, ACAM2000. It’s not going to be used as much for a reason I’ll discuss a little bit later. And then the other one is JYNNEOS that is more recently developed vaccine for it. And it’s usually two injections given four weeks apart.
Alison Werner:
Okay.
Jackie Dorst:
And if someone’s exposed, it could prevent them from having that infection during that window of incubation period, or if they even have a case of monkeypox, it could lessen the symptoms with it. And so it’s a relatively safe virus, not serious side effects. Of course there’s always potential of side effects with any virus, but the ACAM virus has more live viral particles in it, not monkeypox viral particles, but more of the smallpox.
Alison Werner:
Right.
Jackie Dorst:
And so there can be more complications, and you actually develop a pox lesion after having that injection. And there would be a scab form over it. And there’s the risk that with that live viral particles, that if you’re intimately exposed to someone that they could acquire an infection or if their immune compromised. So again, I don’t anticipate unless it becomes a global crisis.
Alison Werner:
Right.
Jackie Dorst:
That we would be using that. So we have treatments. We have a vaccine for it. It can be prevented. CDC has even put up a webpage now because of the sexual transmission on ways to prevent that disease transmission of the monkeypox virus.
Alison Werner:
Okay. Well, let’s go a little more in depth for what the orthodontic team should know as they’re going about their day to keep themselves and their patients safe. I know you mentioned the standard safety precautions. Let’s maybe do a review of that. I know we’ve talked about it many times over the last two years in “In the Sterilization Room,” but let’s do a little review for those who may have gotten a little lax.
Jackie Dorst:
As infectivity has gone down, I’m able to get out and about and be in orthodontic offices more frequently. And in the last four weeks, I’ve been in four offices, almost a hundred employees, doing a mock inspection, and an evaluation and even training with the team. And I’ve noticed that we’ve gotten a little lax.
Alison Werner:
Right.
Jackie Dorst:
It’s our human nature. As the pandemic we feel like is subsiding with it that maybe we’re not as conscientious, let’s say. And I would say as long as you’re wearing your PPE, safety glasses, mask, maybe addition that full face shield when you’re doing aerosol generating procedures and the isolation gown, I think that’s real important ongoing into the future that we’re wearing that gown because we get some splatters and splashes from the patient’s mouth onto a scrub top. And just imagine, how are you going to remove that scrub top at the end of your day in the clinic? You’re going to pull it up over your head, right up your lips, your nose and your eyes.
Alison Werner:
Yeah.
Jackie Dorst:
And if it’s determined that the virus could be transmitted in saliva, that could put you at risk of acquiring an infection through exposure of those mucus membranes.
Alison Werner:
Okay.
Jackie Dorst:
So an isolation gown, you reach behind yourself to untie it, fold it in on itself, remove it, and that’s either disposed of, or it goes to the laundry and normal laundering procedures will destroy.
Alison Werner:
Okay.
Jackie Dorst:
The monkeypox so that’s a safety measure with it, as long as they’re using a healthcare disinfectant, and properly cleaning and leaving that disinfectant wet for the appropriate contact time.
Alison Werner:
Right. Well, also gloves.
Jackie Dorst:
And also gloves. That’s right. With their PPE. Yes.
Alison Werner:
Yeah.
Jackie Dorst:
And very important with that time.
Alison Werner:
Yeah.
Jackie Dorst:
So we’ve got the normal PPE, using a healthcare disinfectant, according to the proper precautions with it, and then also just good hygiene throughout the office. You’re not going to get monkeypox from touching a door handle that somebody’s infected with it. But again, if there’re surfaces that have more contact time, then yeah, we want to be sure certain that we’re using that healthcare disinfectant, and the orthodontic team will be safe with it.
Jackie Dorst:
They should also know what the lesions look like.
Alison Werner:
Right.
Jackie Dorst:
And CDC has provided us with a couple of lesions, one that is on the facial area. Again, it could look like an acne sore that’s healing, and that’s the one that you’re going to be able to pull up on the screen for everybody to see is actually a young adult. He has a light beard with it, and the monkeypox lesion is on his chin. Another is an intra oral lesion that is back in the posterior of the mouth behind the molar area. And it’s very difficult. It doesn’t look like a pox lesion. It could be herpes or an aphthous ulcer with it. It’s very difficult to tell. So if you do have patients that have lesions, obviously you want to be wearing your gloves as you brought up, Alison.
Alison Werner:
Right.
Jackie Dorst:
You don’t want to touch those lesions. You want to stay away from them and do your proper cleaning and disinfection afterwards.
Alison Werner:
Okay. Well, Jackie, thank you so much for this information. I know it will be very informative for the orthodontic teams out there listening. As always we always appreciate your insight, so thank you.
Jackie Dorst:
Well, it’s not always the most exciting or uplifting topics, but it’s something that’s very important for us. And you know, patients have always been aware of how do we have the sparkle in shine in our office? Meaning is it clean? Is it sterile? Is it safe? And after COVID, we saw a very heightened awareness even about the air. Now with monkeypox being in the news, there’s going to be a higher concern.
Alison Werner:
Yeah.
Jackie Dorst:
So it’s definitely the time to reassess the sparkle and shine in your infection control program in your orthodontic practice.
Alison Werner:
Definitely. Well, and to our listeners, I know Jackie mentioned some visuals of the sores. What we will do is we will put those in the show notes. So if you visit our website and look for this podcast episode on the website, you will see the images. And in the meantime, I would say check back soon for the next episode of the Orthodontic Products Podcast. And be sure to subscribe to the MEDQOR Podcast Network in the meantime, to keep up with the latest orthodontic industry news. Visit our website at orthodonticproductsonline.com. Until next time, take care and stay safe.