by Robert L. Waugh, DMD, MS
Ground rules for implementing a diode laser in your practice
-
- Robert L. Waugh, DMD, MS
Diode lasers are finding their way into today’s top orthodontic practices, helping doctors manage common soft-tissue problems associated with patients in braces. Launching this technology safely and successfully depends largely on the orthodontist’s committing time and resources to making an educated purchase, going through training, and developing systems for integrating procedures into the schedule. The following three ground rules greatly facilitate laser implementation and improve the orthodontist’s knowledge, confidence, and enjoyment of the routine daily use of the diode laser.
Ground Rule 1) You Get What You Pay For
A variety of dental diode lasers (DDLs) are available to orthodontists. The costs range from $8,000 to $15,000. The orthodontist must remember that the adage, “You get what you pay for,” is especially true with regard to DDLs.
Since lasers use light energy to perform, specific aspects of this characteristic should be the primary means of deciding which DDL is best-suited for your practice in three areas: wavelength, pulse characteristics, and maximum wattage.
Wavelengths
-
- Three laser wavelengths and their rates of absorption in different compounds.
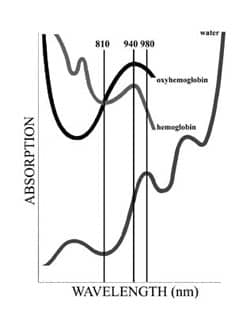
Current DDLs operate in three wavelengths: 810, 940, and 980 nanometers (nm). Each has different effects on soft tissue. The graph (right) shows these wavelengths’ tendencies for absorption in three compounds: hemoglobin, oxyhemoglobin, and water.
An 810-nm laser has the lowest absorption by water of the three categories, allowing for excellent hemostasis during procedures requiring incision and excellent penetration when used at low levels for biostimulation. A wavelength of 940 nm yields the highest overall absorption by hemoglobin, oxyhemoglobin, and water, making this type of laser highly effective for both clean surgical incisions (low carbonization) with excellent hemostasis. A 980-nm laser has the highest absorption by water for clean cutting (low carbonization) with good hemostasis.
Pulse Characteristics
All late-generation DDLs provide laser energy in both continuous wave (CW) and pulsed (P) modes. Continuous-wave laser energy does not allow for thermal relaxation of the tissue, while pulsed modes allow for thermal recovery (cooling) between energy pulses. Importantly, not all pulsing lasers provide energy in the same frequency or duration. In fact, most simply “chop” the laser energy, with energy pulses the same length as rest intervals. This evenly chopped or gated delivery is commonly referred to as a 50/50 duty cycle. In these lasers, the tissue experiences exactly one half the power in P mode as is delivered in CW mode. Consequently, selecting a laser capable of a maximum of 2 W CW will never allow more than 1 W of effective or average power in P mode.
Average power is important because most soft-tissue procedures performed with DDLs require between 1 and 2 W of power. In other words, the P mode of a 2-W or 3-W laser will not deliver the amount of energy necessary to cut heavily fibrous tissue, requiring the orthodontist to revert to CW mode to complete the procedure. In these instances, the tissues are inevitably more prone to thermal damage and charring, absent the cooling periods between pulses. Thermal damage has implications for patient comfort, both during the procedure and during postoperative healing.
Variable pulse modes available with some lasers are necessary for the orthodontist who enjoys delivering a more refined surgical and postsurgical experience for patients. The most sophisticated DDLs alter the delivery ratio of laser-firing time to cooling or recovery time. For example, the “comfort pulse” mode on the ezlase 940 allows the laser to fire for .05 milliseconds and then gives the tissue 0.20 milliseconds to cool, for a 1:4 ratio. Lasers without variable pulse capabilities typically deliver 20-millisecond pulses (400 times longer) with equal thermal recovery times, resulting in overheated tissues. The 1:4 energy ratio has been shown to result in transient elevations in tissue temperature too low to induce injury. In my practice, I see little to no charring when performing postorthodontic soft-tissue recontouring using 0.05-millisecond laser pulses and 0.20-millisecond rest intervals. Thermal relaxation times of 0.15 to 0.20 milliseconds are critical to keeping internal tissue temperatures within biologically viable parameters.
Most impressive about DDLs with a wide range of selectable pulse settings is that they can usually be used without anesthesia due to the nature of laser energy used with rest intervals.
Maximum Wattage
A DDL’s maximum wattage affects how much effective or average wattage can be delivered to the tissue—extremely important when using pulsed modes. For example, a DDL with a maximum 2 W of power delivering pulse lengths equal to pulse intervals (50/50) delivers an average power of 1 W. Why is this important? With a labial frenectomy, my experience has been that an average power closer to 1.8 W is needed to cut the tough, fibrous connective tissue found internally. While the laser could be used in CW mode, the energy would char the tissue, resulting in the need for anesthesia as well as greater postoperative discomfort and scarring—components commonly seen with electrosurgery.
On the other hand, a DDL delivering a greater maximum wattage with adjustable pulses can provide average wattages kinder to the tissues. For example, a 0.10-millisecond pulse with 0.20-millisecond rest intervals delivers just 33% of the maximum selected power. To deliver the average 1.8 W needed to cut fibrous connective tissue in this P mode, you need a maximum wattage of 5.6 W.
A final aspect of, “You get what you pay for,” is training. If a manufacturer includes training with the purchase of a laser, ask if it includes live instruction, if it is specific to orthodontics, and if it includes patients in the course. As evidence of competency, such a course would carry great weight. Even better would be attending a course recognized by an accredited entity of continuing dental education credits.
In 1993, the Society of Photo-Optical Instrumentation Engineers published guidelines to help ensure that dentists using lasers are properly educated about safety. At the least, a new user should attend a course that satisfies the guidelines’ “Standard Proficiency Course” definition, with both didactic and hands-on experiences as well as safety assessments in both; from a medicolegal standpoint, it is only prudent.
Ground Rule 2) Safety First
DDLs are medical devices regulated by the FDA for good reason: They emit dangerous levels of laser radiation. Keep in mind that the beam is a tightly collimated ray of energy capable of destroying soft tissue. For example, the vascular retina is hemoglobin-rich. Transient exposure to a DDL beam can cause irreversible harm, even instant blindness. All of the safety engineering in DDLs helps ensure patient safety, but only if the orthodontist and staff are fully knowledgeable about them.
The Occupational Safety and Health Administration (OSHA) focuses on employees exposed to the laser in their everyday work lives. Three components ensure maximum safe operating procedures: personal protective equipment (safety glasses), adequate training, and treatment-area modifications.
Eye Protection
Without question, eye protection is paramount. No one must be in the treatment area when the dental laser is in use unless they are wearing the correct safety glasses. “Correct” safety glasses have proper filtration to the specific wavelength of laser light. Laser safety glasses are not transferable among various wavelengths.
OSHA states, “You must provide safety goggles specifically designed to protect the employees’ eyes from the specific intensity of light produced by the laser …. If your employees are exposed to laser beams, you must determine the maximum power density, or intensity, that the lasers can produce … and select lenses that will protect against this maximum intensity.”
Based on power output, divergence, and beam configuration, a nominal ocular hazard distance can be assessed. This is the distance from the laser emission beyond which the eye risk is below the maximum permissible exposure level. For a Class IV dental laser, it is approximately 10 feet.
Finally, the orthodontist must also wear eye protection. If you use magnifying loupes in practice, special filters that fit inside the lenses can be purchased. Ultimately, the person who has the responsibility of turning on the laser and making sure all the safety features are operational during the process must also be responsible for proper laser eye protection.
Training and Documentation
Someone within the practice must be designated the laser safety officer (LSO). This person is trained to monitor and enforce the overall laser safety program, which includes the following:
- Confirming the classification of laser used;
- doing the nominal hazard zone evaluation;
- ensuring that proper control measures are in place and approving substitute controls;
- approving standard operating procedures;
- approving eyewear and other protective equipment;
- posting special appropriate signs and labels and overall facility controls; and
- effecting proper laser safety training.
The LSO ensures that employees assigned to work around laser equipment are appropriately qualified and trained. The names of all persons trained and the date of training should be documented.
Training is specific to the FDA classification of the DDL in use; most DDLs are Class IV (meaning they have a continuous wave greater than 500 MW). Training begins with the information contained in the operation and maintenance manuals of the laser, along with additional basic safety literature. I recommend additional training that provides a complete understanding of the requirements of a safe laser environment, including discussions of hazards, safety devices required, procedures related to equipment operation, warning sign requirements, and descriptions of medical surveillance practices, with emphasis placed on practical, safe laser techniques and procedures, as well as on devices that provide a safe environment.
-
- This series of images shows how a diode laser can help with bracket placement on a bicuspid.
Treatment-Area Modifications
Class IV lasers are hazardous to view either directly or diffusely scattered, and are potential fire and skin hazards. The American National Standards Institute requires posting areas where Class IV lasers are in use with the DANGER sign.
The absence of reflective materials in the laser use area ensures beam containment. In addition, high-volume evacuation must be used to remove the laser plume, which could be laden with viral particles. Using the laser in the open-bay environment of orthodontics is not recommended unless all persons wear protective eyewear and adjacent reflective surfaces are covered.
Ground Rule 3) Communication Is the Key
An important component of smoothly integrating a DDL into practice is communication to patients, dentists, and neighboring specialists. Obtaining a patient’s informed consent is often an obstacle for new orthodontic laser users. It is the doctor’s responsibility to use forms to properly document informed patient consent. Manufacturers’ training may provide a template for the doctors to adapt for practice; private vendors also provide them. Whatever the source, the forms should be reviewed and approved by legal counsel before you use them. I found that adding the laser language to my conventional informed consent form works well, since I consider laser procedures an integral part of my orthodontic practice.
Properly describing newly available laser services to referring dentists, as well as to local periodontists and oral surgeons, is equally important. Be proactive and up-front. DDLs benefit orthodontic patients through shorter treatment times, better hygiene access, and improved aesthetics. Let the doctors know firsthand you are providing laser services, and explain why. Expect some backlash. You might find a few periodontists have not accepted dental lasers as viable treatment options. Do not allow a “doubting Thomas” to keep your patients from benefiting from a proven treatment entity.
Consider a mailing to your fellow dentists, explaining the laser you use and why—emphasizing orthodontic uses. Hold a Saturday-morning “open house” where you explain how the laser helps patients every day in the ways mentioned above. Refrain from becoming defensive if challenged about “stepping on periodontists’ toes” or of using a laser to “pad the bottom line.” You will find that DDLs play a major role in kinder patient care. For example, they allow routine laser-facilitated access for bracket placement without the drama of intravenous sedation and referral to another doctor. Patients and parents will love you for it, and that is what matters most.
Ground Rule 4) Baby Steps
Introducing a laser to your practice means taking a series of “baby steps” to ensure everyone’s safety and satisfaction. These steps include laser selection, establishing your limits, scheduling, and anesthesia.
Laser Selection
You probably have some idea of the DDLs available and how to select one. Consider factors like anesthesia: Will you routinely administer local anesthesia in your practice? Some DDLs will require it; others will not. Will you whiten teeth? I do not recommend doing that, out of respect for referring dentists. However, if you do want to use a DDL for whitening, consider the 810-nm version. For daily soft-tissue procedures in orthodontics, a 940- to 980-nm DDL works best.
Know Your Limits
Here is a personal story that ended happily. A doctor who was scheduled to be present and train me the first day I used a dental laser, did not show up. My patient was scheduled for a lingual frenectomy. With an educational DVD in my laptop, I felt confident and decided to proceed. Imagine my surprise when the DVD’s narrator said, “Do not attempt a lingual frenectomy as your first procedure. …” Well, I did, and the results were tremendously gratifying to me, the patient, and his parents.
The range of FDA-approved DDL soft-tissue procedures is extensive, but certain ones will dominate your practice: gingivectomy for bracket placement, aesthetic gingival recontouring, frenectomy, fibromotomy, and opeculectomy. Occasionally, you might expose a palatally soft-tissue-impacted tooth to facilitate eruption.
Considering the list of potential procedures, I recommend that you begin your laser career with procedures you feel most comfortable with. Keeping in mind the vascular-rich area beneath the tongue, I trust it will not be a lingual frenectomy!
Scheduling
At first, consider setting aside “laser days” for your initial procedures. Schedule an hour per procedure, allowing you and the staff to prepare for each. Eventually, you will routinely include laser procedures in your scheduling template, with the staff trained to have the patient ready.
Anesthesia
Some laser procedures require no anesthetic, while others require local anesthetic infiltration. Dental lasers have significant favorable neuropharmacologic effects on the synthesis, release, and metabolism of histamine and prostaglandin, on decreased c-fiber activity, bradykinin release, and favorably altered pain thresholds. Patients often do not differentiate nonpainful sensations from overt pain, so you should be proactive about not allowing any chance of pseudopain sensation that might spiral the patient into a state of anxiety, releasing endogenous chemicals that local anesthesia might not eliminate. I use topical anesthesia on all of my laser patients.
A topical known as TAC-Alternative (“TAC” stands for tetracaine, adrenaline, cocaine) works well, providing up to 2.5 mm of deep anesthesia, adequate for most laser procedures. The onset is 3 minutes, and duration is as long as 20 minutes. If possible, the medication can be placed beneath an operculum to facilitate the procedure. TAC-Alternative is a thick, proprietary gel sold in 20-g light-protected jars and is made from 20% lidocaine, 4% tetracaine, and 2% phenylephrine.
When a topical anesthetic is inadequate, a local anesthetic may be needed. Refrain from those with a vasoconstrictor, which may impede the ability of the laser to act on the needed hemoglobin pigmentation.
Ground Rule 5) It’s in the Details
Of course, how you manage your laser fees, bill your patients, and help with insurance is up to you. The simplest method is using a superbill with commonly used procedures, letting the patient file for reimbursement. You will probably not charge for procedures that make your job easier, such as a gingivectomy to facilitate bracket placement.
Here are some simple guidelines to help minimize problems:
- Create and use a laser consultation sheet that includes procedure, tooth number(s), etc.
- Probe all cases, chart, and submit for insurance.
- Use the latest CDT codes, as published by the ADA.
- Research fees and charge in the 95th percentile.
- Never discount periodontal procedures in a way that might undercut periodontists’ fees.
Complete OSHA guidelines regarding laser safety can be found at www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=DIRECTIVES&p_id=1705.
Robert L. Waugh, DMD, MS, is an assistant professor at Medical College of Georgia, where he introduced lasers into the orthodontic residency program. He was the first orthodontist to present applications of the YSGG Waterlase and diode laser at the 2005 WCLI Super Symposium. He is a member of the International College and American College of Dentists, an ABO Diplomate, and a member of the Academy of Laser Dentistry. He is the owner ofintelliDENT, which provides training for new ezlase diode laser users. He can be reached at