by James M. Broadbent, DDS, MS
What an orthodontist can do to ease the pain
Last week during a family dinner, my nephew, a young orthodontist, asked me, “What do you do to treat TMJ (temporomandibular joint disorder) patients?” He said, “I can help a few people with braces, but not most. I have tried to treat some patients with splints, but I have no idea what type to use. I refer my patients with jaw problems, but it is frustrating to have a dentist treat with a splint and then refer back with instructions to stop the splint and do orthodontics. What am I to do?” This orthodontist is not alone. I dare to bet that you, too, have experienced such a quandary.
An orthodontist in my study group commented, “I do orthodontics. Why should I have an interest in TMJ? My interest is in helping individuals enjoy straight teeth and a beautiful smile. When the teeth are straight and the bite is corrected, don’t the jaws work OK?” Maybe yes, maybe no—it depends!
My orthodontist friend asked, “Why are you so concerned about the jaw joints? I, like you, do orthodontics, but my patients do not have jaw problems. Why would so many of your patients have jaw problems?” Could it be my colleague was not aware of preexisting jaw conditions and therefore was not looking for them or asking discovery questions? Given limited space, this article will present TMJ in the orthodontic office.
Abnormal or Malformed Jaw Joints
You can perform a simple clinical test by using a ruler to measure range of jaw motion and your fingers to palpate the temporomandibular joints. A range of jaw motion for healthy jaw joints is 45 to 55 mm interincisal vertical and 9 to 13 mm lateral.1Brendan Stack, DDS, MS, considers 48 mm to 60 mm vertical to be the standard clinical goal. Jaw opening should be pain-free, smooth, uninhibited, and symmetrical, without deviation or deflection, clicking, or locking. When it is not, then something is wrong. The range-of-jaw-motion test is recommended to be routine in the clinical examination and treatment-progress chart entry.
Michael Alpern, DDS, MS, published a statement that may not be causally set aside. “Teeth and jaws affect the TMJs, TMJs affect the teeth and jaws. Orthodontics affects both … If a patient presents with dysplasia or malformation of the teeth and jaws (and that patient has been functioning on those malposed teeth and jaws), you cannot assume that the patient’s TMJs are normal. Usually, the TMJs may also be abnormal and/or malformed.”2Altered function and muscle overload are thought to be contributing factors to the distortion of cranial bones and dental malalignment.
The above statements deserve the orthodontist’s full attention and must be reckoned with. The quote may beg to differ with an official position paper stating that there is no relationship between malocclusion, orthodontics, and TMJ disorders. Perhaps an interpretation may be that an individual may have perfectly well-aligned teeth and a dysfunctional jaw joint, or possess the worst-possible misaligned teeth and have an accommodated, healthy jaw joint. A caveat is to differentiate between signs and reported symptoms and the presence or absence of a TMD. Patients may have adapted to an internal derangement or degenerative joint condition and function with no reported symptoms. To diagnose condyle-fossa-disc function, radiographic imaging of both TM joints and a submental vertex (SMV) film is recommended to be part of the standard orthodontic-records protocol.
Many factors may predispose an individual to a jaw disorder. A University of Illinois study reported that more that two thirds of patients presenting to the clinic had pretreatment signs or symptoms of TMD. A higher percentage was reported following orthodontic treatment. The study was repeated at the University of Rochester with similar results. Thus, one may conclude that orthodontic treatment did not resolve TMJ for most patients. Early in my orthodontic career I determined from personal experience that conventional orthodontics helped only a few TMJ patients. Most did not improve, and many reported an increase of jaw symptoms following my best orthodontic care. Something other than orthodontics is needed to get another outcome.
 |
 |
 |
 |
Internal Deranged Jaw Joints
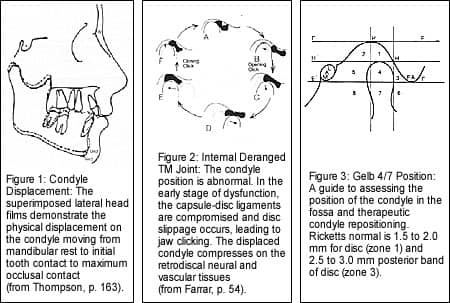
John Thompson, DDS, MS,3one of my professors, taught how skeletal and dental structural conditions may be factors associated with the onset and perpetuation of certain jaw disorders. Differential growth of the mandible may be impeded by upper-jaw conditions such as spatial asymmetry of the maxilla, narrow width, and crossbite. Also, incisal misguidance has been identified to be a major factor in TMDs. Malpositioned incisors may interfere with the neuromuscular path of closure from mandible rest position to initial incisal contact to maximum intercuspation (Figure 1, page 18). Abnormal muscle function and structural conditions may proprioceptively and mechanically interact, causing the adaptive mandible condyles to become posteriorly and superiorly displaced at maximum intercuspation. The altered joint loading and dysfunction microtrauma may result in capsular ligament damage and anteromedial disc displacement. With time, the degenerative process may progress to varied stages as host conditions allow.
Farrar and McCarty4report that about 25% to 30% of the population have internal derangements. However, they estimate that 93% of patients presenting to their TMJ offices have internal derangements (Figure 2, page 18).
In the early teens, the most common symptom of TMJ is clicking. As the incidence of clicking decreases, the incidence of locking increases, and so does degenerative arthritis. Around the age of 40, the incidence of clicking, locking, and degenerative arthritis is about equal. After 40, clicking and locking decrease, and the incidence of degenerative arthritis increases. Overall, TMD conditions tend to become worse with time.
Signs and Symptoms of Jaw Disorders
Dysfunctional loading of the TMJ capsule and the retrodiscal tissues results in degenerative change, and a myriad of seemingly unrelated symptoms may ensue.
All too often, relief is sought for a given symptom without addressing the root cause. The symptoms may be masked with therapy or medication, only to return when the prescribed agent is discontinued. This may be disconcerting to both the patient and the physician.
Someone labeled TM disorders “the great mimicker.” The trigeminal nerve is the largest cranial nerve. It has the ophthalmic, upper-jaw, and lower-jaw major branches. The autonomic nerve system is closely associated with the trigeminal tract. Neurovascular headaches as well as localized and referred pain patterns are associated with these nerves. Internal derangement and chronic pain cause neurological input overload. Is it any wonder why the signs and symptoms of TM disorders may be so diverse?1,5–8
The Orthodontist
What does this have to do with orthodontics? Simple. Orthodontic procedures are optimally done on individuals with healthy jaw joints. However, patients presenting for orthodontic procedures have a high probability of internally displaced joints. Alignment of the teeth in the presence of a pathological joint condition does not help the jaw condition and tends to lock in the condition. A clinical guide is the following: Whenever possible, establish a pain-free, symptom-free, and normal position of each condyle and disc in the TM fossa before orthodontics.
The aware orthodontist has an opportunity to address TMD and improve the quality of life for his or her patients by doing a few things differently before or concurrent with conventional orthodontics. The majority of individuals with internal derangement and associated craniofacial pain will respond favorably to orthotic and functional jaw orthopedic-appliance therapy.
What is needed is a tooth-borne acrylic splint constructed to the level of initial incisor contact to prevent overclosure of the jaws and allow for physiologic recapture of the condyle-disc assembly to restore and maintain mechanical best-possible function (Figure 2, page 18). A subtle orthotic modification with profound effect is to increase the posterior vertical built into the provisional diagnostic appliance. The Gelb 4/7 position (Figure 3, page 18) is a clinical guide to splint construction. It is critical that the superior joint space be about 3+ mm for disc recapture.
Often, a functional mandibular-repositioning appliance is needed to recapture the disc and stabilize the temporomandibular disc assembly and the mandible to the cranium. In many situations, the maxilla needs to be expanded and the incisor teeth need to be moved to allow for physiologic positioning of the mandible for TMJ purposes. Parenthetically, in Class II malocclusions, as the jaw is repositioned for TMJ purposes, the teeth go along for the ride toward a Class I relationship. However, Class I malocclusions with underdeveloped maxillae and “trapped mandibles” tend toward Class III.
Case Study
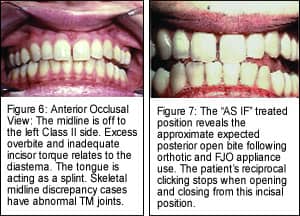
The patient had prior orthodontics with a very competent orthodontist. Take notice of the presenting Class II, subdivision left, malocclusion (Figures 4 to 6, page 20). Skeletal midline discrepancy cases usually have abnormal TMJs. With disc displacement, the bite changes. She was seeking secondary treatment for relapse of the upper diastema and specifically for relief of chronic headaches in the cervical, frontal, and temporal regions, as well as localized pain over the jaw joints. Reciprocal clicking was present in both joints and was more intense on the left side.
This case is representative of a patient with an early reciprocal click. As the jaws open, a click is experienced in the 25-mm range. Once the disc or discs are recaptured, the patient can then open and close smoothly (Figure 7, page 20). When the teeth again are occluded in maximum intercuspation, the discs are again displaced and clicking returns. Plastic is the secret to treating TMJ. Placement of a diagnostic orthotic to reposition the mandible downward and forward with skeletal midlines aligned will most likely recapture the discs, stop the clicking, and reduce facial pain. If so, the occlusion may be altered with orthopedic, orthodontic, and/or prosthodontic procedures to stabilize the bite jaws.
The low frenum attachment, improper upper-incisor torque, lateral tooth size, and overbite are factors in the diastema (Figures 8 and 9). Removal of the labial frenum and orthodontic retreatment may close the diastema. It is possible to distally move upper molars, again close the diastema, and adjust the bite with orthodontics, and not address the jaw condition. To do so would most likely exacerbate the pretreatment jaw condition. This would be contraindicated. Clearly more than orthodontic procedures are needed.
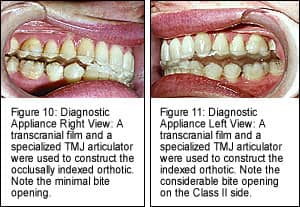
Diagnostic Appliance
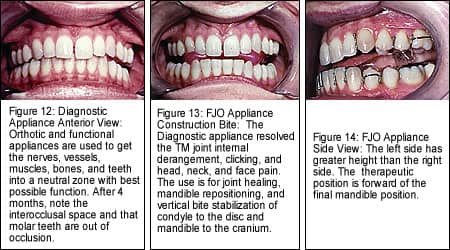
The transcranial joint images reveal the condyle to be displaced posteriorly and superiorly in both joints, more so on the left. The condyles were compressing upon the retrodiscal tissues, and the discs were medially displaced. The transcranial joint films were used to calibrate a specialized articulator. A provisional construction bite was made on the mounted models. The bite was seated in the mouth, and another film was taken to confirm Gelb 4/7 position (Figure 2, page 18). When acceptable, the case was shipped to the laboratory for diagnostic appliance (orthotic) construction (Figures 10 to 12, pages 22 and 23). The diagnostic appliance relieved all head, as well as neck pain and clicking of both jaw joints.
Orthopedics
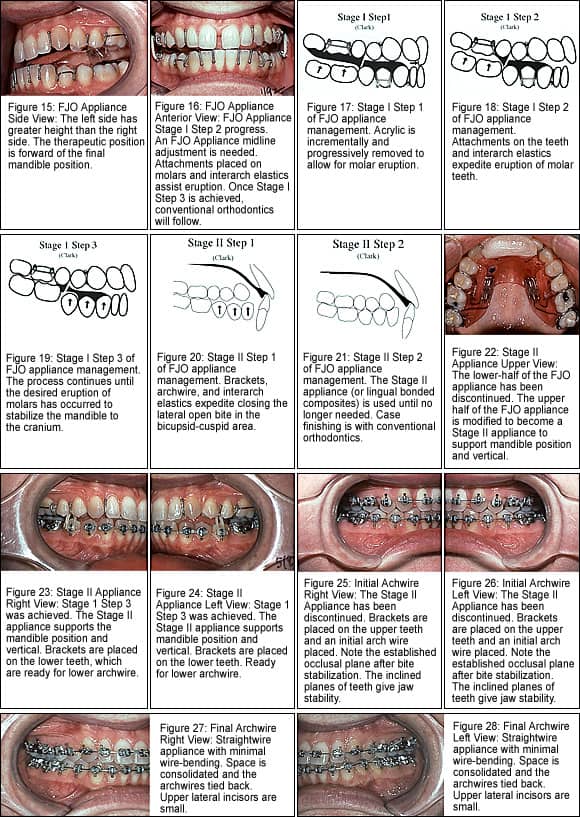
To reposition the mandible and facilitate bite stabilization, a functional appliance was selected. There are many methods to achieve bite stabilization. I decided to use a Broadbent-modified Clark9 two-piece functional jaw orthopedic (FJO) appliance constructed to the diagnostic appliance position (Figures 13 to 15, page 23*).
Bite Stabilization
In most cases (not all), posterior interocclusal space is expected with use of TMJ mandible-repositioning splints and functional jaw orthopedic appliances. Note the patient’s interoccclusal space and the difference between the right and left sides. It represents the degree of abnormal compensaton in the jaws and dental structures. The limitation of conventional orthodontics in treating TMJ conditions is evident. Most orthodontists do not understand the collapsed, vertical-overclosure condition associated with posterior lateral open bite.
To stabilize the mandible to the cranium and maintain jaw function, the space is closed with molar-controlled vertical eruption. Bite stabilization involved attachments on posterior teeth and the use of interarch elastics along with the two-piece FJO appliance (Figure 16*). Significant leveling is needed. Once Stage I Step 3 was achieved, the patient had occlusal contact on the right and left molars and incisors (Figures 16 to 19*). The lower part of the FJO appliance was discontinued and the upper part was intraorally modified to be a Stage II appliance (Figures 20 to 24*). From here, conventional orthodontics follows.
Orthodontics
Because a Class I dental and skeletal relationship has been established and the jaws’ function is now normal, orthodontics is expected to be straightforward and the outcome stable (Figures 25 to 28*).
Orthodontic root paralleling, positioning of crowns, and torquing were routine. The arches were consolidated, and Andrews Six Keys to Optimal Occlusion were met. The range of jaw motion was within normal limits.
Retention
In this case, retention was a lower lingual and upper removable retainer. The case is stable after more than 14 years. Often in TMD cases, a one-piece FJO appliance is used for jaw-repositioning maintenance. In this case, the FJO appliance was not used for TMJ maintenance purposes.
In summary, the aware orthodontist has an opportunity to address TMD and improve the quality of life for his or her patients by doing a few things differently before or concurrent with conventional orthodontics. The application of orthotic and functional jaw orthopedic-appliance therapy principles as presented addresses the root cause and will help the majority of individuals with internal derangement and associated craniofacial pain in the orthodontic practice.
James M. Broadbent DDS, MS, maintain a private practice in Provo, Utah. He is a diplomate of the American Board of Orthodontics and a diplomate of the American Academy of Pain Management. He can be reached at [email protected].