with Jon D. Holmes, DMD, MD, FACS

Holmes: E-mail has become the main communication avenue for many of my main referrals. This has become especially helpful in directing the placement of temporary orthodontic anchors. A doctor can e-mail a picture, and mark the proposed placement site for me. That being said, I never hesitate to pick up the phone if there is any question about the treatment plan. I really appreciate written instructions when it comes to extraction plans.
I think that it is incumbent on the surgeon to open a communication with the orthodontist and engage them in the treatment-planning process. If goals are not set at the outset, the result can be less than optimal. A classic example is transverse deficiency of the maxilla. If the oral and maxillofacial surgeon is planning a two-piece lefort osteotomy, and the orthodontist is not aware of that, then the orthodontist may expand the teeth during the pre-surgical phase of ortho. Following surgery, relapse of the dental movement can result in an open bite. Also, an orthodontist can really help the surgeon out in the early post-operative setting. Teeth move very quickly following surgery, and properly applied mechanics can keep a small problem from becoming a big one.
OP: What is the worst thing an orthodontist can do in working with an oral surgeon?
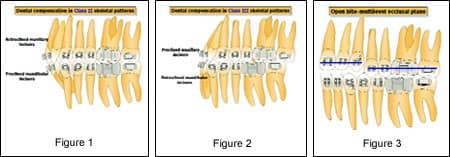
Holmes: In a Class II patient, failure to upright the lower incisors can result in an inability to advance the mandible enough to obtain a Class I relation of the buccal segments (Figure 1). Class III elastics in the preparatory phase can help. Extraction of lower bicuspids may or may not be needed depending on the amount of crowding and incisor proclination. We are, however, removing fewer lower first bicuspids, especially in females, where the amount of incisor uprighting can lead to overadvancement of the mandible. An alternative may be to remove second bicuspids in borderline cases. Similarly, in Class III cases with significant concavity of the facial profile, if the lower incisors are incompletely decompensated in the presurgical phase, there may be inadequate space to advance the maxilla (Figure 2). In severe cases, Class II elastics in the preparatory phase can maximize the aesthetic outcome. The orthodontist and surgeon also need to make a decision early in treatment regarding the need for multisegment orthodontic alignment and osteotomies of the maxilla. If aggressive leveling of a significant curve of Spee occurs in open-bite cases, relapse of the open bite may occur post-operatively. Segmental mechanics can help with this (Figure 3). Finally, I am discouraged when I see patients that present for consultation after having bicuspids extracted in an attempt to avoid surgery, and then a decision is made to consider surgery. That can present some difficulties. I believe patients and their families should be counseled thoroughly about the alternatives, including surgery, at the outset. If there is doubt, have the patient see an oral and maxillofacial surgeon to hear the surgeon’s side. That allows good informed consent.
Jon D. Holmes, DMD, MD, FACS, has a private practice in Birmingham, Ala. He is board certified by the American Board of Oral and Maxillofacial Surgeons. He can be reached via e-mail at [email protected].









