by Dipak Chudasama, BDS, MSC, MORTH RCS, and Laurance Jerrold, DDS, JD, ABO
A clinician’s guide to space closure using nickel titanium coil springs
 |
 |
| Dipak Chudasama, BDS, MSC, MORTH RCS | Laurance Jerrold, DDS, JD, ABO |
There is little agreement in orthodontics about which method of space closure is the most efficient. The best method of space closure chosen should have the highest amount of tooth movement with the least amount of destruction to the periodontal ligament, alveolar bone, or root.1 Ideally, orthodontic tooth movement should be the result of light, continuous forces for optimum tissue response and rapid tooth movement.2 Storey showed that light, continuous forces ranging from 75 g to 100 g achieved tooth movement in the range of 0.5 mm/week.3 For reciprocal space closure, it has been suggested that a force of 100 g to 200 g is needed when using straightwire appliances.4 Over the years, a variety of materials have been used to close spaces between teeth. These include elastic modules of various sorts,5 elastomeric chain, and stainless steel and nickel titanium (NiTi) springs.6
Coil Springs
Coil springs date back to 1931, when they were first used for tooth movement.7 The two types of springs used clinically are open- and closed-coil design. Some of the factors that affect a spring’s force level include the following: the type of alloy, the wire size, the lumen size, the pitch angle of the coils, the distance the spring is stretched, and the length of the spring.8 The load-deflection rate increases in coil springs as wire size and pitch angle increase.9,10 The pitch angle is the angle between the coils and perpendicular to the long axis of the spring. On the other hand, the load-deflection rate decreases as lumen size and spring length increase.11
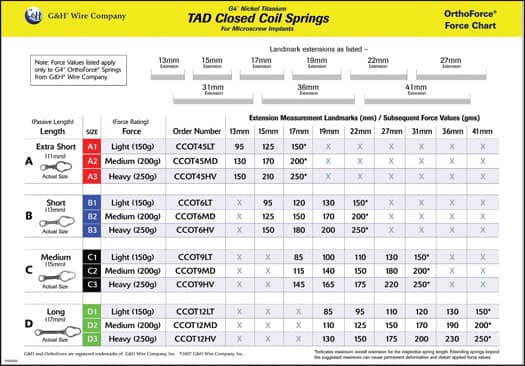 |
| Using this chart can help orthodontists determine and apply various force levels. |
Dixon et al also compared the clinical effectiveness of NiTi springs, elastomeric chains, and elastic modules. Their study showed that space closure for the three different methods was: 0.81 mm, 0.58 mm, and 0.35 mm.11 Nagamoto suggested that the “pulling action” delivered by closed-coil springs is more delicate, and that such a force is desirable during the course of orthodontic treatment.12 Orthodontic coil springs have primarily been made of stainless steel and cobalt-chromium-nickel (Co-Cr-Ni) alloys. However, NiTi coil springs have recently been introduced and are suggested to have better springback and superelastic properties than stainless steel coil springs.13
The advantage of NiTi springs over elastomeric chain or active modules is that their force does not decay significantly over time.14,15 In general, coil springs have shown an 8% to 20% force loss at the end of 28 days, which is much less than the force decay of natural latex and synthetic elastic modules.7 Moreover, NiTi springs have been known to give quick and consistent rates of space closure.16–18 NiTi springs have been shown to give the most rapid rate of space closure, and may be considered the treatment of choice.18
Clinical Application
Recently, G & H Wire Co introduced the OrthoForce® Force Chart (page 54), which details the force values achieved based on the different extensions of NiTi space-closing coil springs. Using that company’s coil springs and the force level chart, you can determine and apply various force levels from as little as 30 g to as much as 250 g. Coil springs are available for both conventional space closure and for use with temporary anchorage devices. Both the 9-mm and 12-mm lengths are available for the traditional closed-coil spring, and each length has five different force levels to choose from. There are four lengths of TAD closed-coil springs, with three force levels in each type.
In summary, NiTi closed-coil springs are often misinterpreted as having constant force no matter what the extension. There is no such thing as a constant-force spring, so the amount of extension is clinically significant. Force graphs for elastomerics (rubber bands) have already been developed.19 Armed with this information, contemporary orthodontists have at their disposal easy methods to assess the correct force-generating module—be it a rubber band or a coil spring—that will yield the exact force levels to fit the clinical situation presented by the patient. Utilizing appropriate force levels is one of the keys to achieving successful, reproducible, and predicable orthodontic results.
Dipak Chudasama, BDS, MSC, MORTH RCS, is an assistant professor and the director of research at the Jacksonville University School of Orthodontics. He can be reached at
Laurance Jerrold, DDS, JD, ABO, is the dean and program director at the Jacksonville University School of Orthodontics. He can be contacted at
References
- Pilon JGM, Kuijpers-Jagtman AM, Maltha JC. Magnitude of orthodontic forces and rate of bodily tooth movement: An experimental study. Am J Orthod Dentofac Orthop. 1996;110:16-23.
- Angolkar PV, Arnold JV, Nanda RS, Duncanson MG Jr. Force degradation of closed coil springs: An in vitro evaluation. Am J Orthod Dentofac Orthop. 1992; 102:127-133.
- Storey E. The nature of tooth movement. Am J Orthod. 1973;63:292-313.
- Quinn RS, Yoshikawa DK. A reassessment of force magnitude in orthodontics. Am J Orthod. 1985;83:252-260.
- Samuels RHA, Rudge SJ, Mair LH. A comparison of the rate of space closure using nickel-titanium spring and an elastic module: A clinical study. Am J Orthod Dentofac Orthop. 1993;103:464-467.
- Dixon V, Read MJF, O’Brien KD, Worthington HV, Mandall NA. A randomized clinical trial to compare three methods of orthodontic space closure. J Orthod. 2002;29:31-36.
- Anderson GM. One use for the Arnold coil spring. Int J Orthod. 1931;17:688.
- Boshart BF, Currier GF, Nanda RS, Duncanson MG Jr. Load deflection rate measurements of activated open and close coil springs. Angle Orthod. 1990;60:27-32.
- Born HS. Some facts concerning the open coil spring. Am J Orthod. 1955;45:917-925.
- Kobayashi K, Muramatsu A. Mechanics of orthodontic springs. J Jap Stomatol Soc. 1972;39:1-15.
- Webb RI, Caputo AA, Harvy K. Orthodontic force production by closed coil springs. Am J Orthod. 1978;74(4):405-409.
- Nagamoto G. Contraction coil springs: its uses and how to make it. Am J Orthod Oral Surg. 1947;33:392-395.
- Miura F, Masakuni M, Ohura Y, Karibe M. The super-elastic Japanese NiTi alloy wire for use in orthodontics. Part III. Studies on Japanese NiTi alloy coil springs. Am J Orthod Dentofac Orthop. 1988;94:89-96.
- Rock WP, Wilson HJ, Fisher SE. Force reduction of elastomerid chains after one month in the mouth. Br J Orthod. 1986;13:147-150.
- Kuster R, Ingervall B, Burgin W. Laboratory and intraoral tests of the degradation of elastic chains. Eur J Orthod. 1986;8:202-208.
- Samuels RHA, Rudge SJ, and Mair LH. A comparison of the rate of space closure using nickel-titanium spring and an elastic module: A clinical study. Am J Orthod Dentofac Orthop. 1993;103:464-467.
- Samuels RH, Rudge SJ, Mair LH. A clinical study of space closure with nickel-titanium closed coil springs and an elastic module. Am J Orthod Dentofac Orthop. 1998;114:73-79.
- Sonis AL. Comparison of NiTi coil springs versus elastics in canine retraction. J Clin Orthod. 1994;28:293-295.
- Chudasama D, Long R, Jerrold L. The truth about stretching. Orthodontic Products. 2008;15(6):32-34.










