by Michael C. Alpern, DDS, MS
How clear plastic aligners can help perfect cases

Michael C. Alpern
When I am examining a patient, I wear magnifying loupes with a xenon light. I always try to complete my banded/bonded orthodontic treatment as perfectly as I can, but after removing all bands and bonds and making models, I sometimes find surprises.
Looking at the “retention models,” I may find that the 3D views of the models bring to light a small space I missed, a molar torque that is inadequate, or other small finishing needs. To make retainers would retain these small problems.
However, today’s technology permits me to make aligners that I call “finishers” prior to making retainers. From an informed consent standpoint, my practice now informs patients that several months of clear, flexible finishers may be used between removal of braces and making retainers. This is a technique first described by Keith Hilliard, DMD, of Lakeland, Fla.
Starting to Finish



Figure 1: In this case requiring finishers, we marked the initial model (A) with lingual divots (B) created with a 6 round bur in a laboratory handpiece. We then light-cured Triad liquid acrylic to create the space for the tooth to move into (C).
After removing brackets and bands, I examine each set of completed models. If I find a small correction that would improve my result, I plan for finishers.
Using an 8 or 6 round bur in a laboratory handpiece, I make small divots where I need force applied. Using Triad liquid acrylic (from Dentsply), we create space for the tooth to move into. It is important to make sure the tooth has room to move at the incisal or occlusal. Then, using heat-pressurized or suction machines, we process clear, flexible .040-inch sheets over the “corrected” model.
Choosing the clear, flexible sheets to be processed over the models is important. For example, the completed surface of the finisher should be slick and smooth. This encourages smooth clenching by the patient without deflecting abnormal mandibular movements. Materials lacking smooth surfaces can cause traumatic deflections of mandibular closing movements. Any encumbrances to freedom of mandibular motion can potentially result in permanent damage to the fragile temporomandibular joint fibro-cartilage of the disc and the lining of the condylar fossa and articular eminence.
The technology of the machines forming these appliances and the science and chemistry of the materials have made significant progress in the past few years. Several machines heat evenly and can exert up to six atmospheres of pressure or suction. This compression or suction can remain on during cooling, which helps eliminate warpage. The chemistry of materials has also reduced distortion or warpage during cooling.
Once the heating, compression or suction, and cooling are completed, we use double-action scissors to do the large trimming. We then use diamond discs to trim the margins of the appliances. It is important to eliminate soft-tissue undercuts or any areas where soft-tissue compression might unintentionally occur. Cone-shaped polishers made of silicone, mounted on laboratory mandrels (from BrasslerUSA) and used in laboratory handpiece units, make marginal finishing more exact and result in smooth edges. Unlike traditional laboratory acrylic burs, these innovative cones eliminate the risk of catching edges and cutting in the wrong direction. New mandrel-mounted brushes help polish and eliminate small, ragged edges.
The resulting finishers are clear, flexible, and comfortable. If worn full-time (except for eating), they can make final finishing more satisfying for patient and orthodontist.
Limitations of Finishers
Finishers can only provide small amounts of tooth movement at one time, using a single appliance. Trying to move a tooth more than 1 to 2 mm invites failure. Therefore, additional tooth movement requires a new finisher.
Excessive divoting or a buildup of Triad liquid acrylic can make the appliance difficult to seat. Patients object to trying to bite down on the appliances full-time for several days to complete seating.
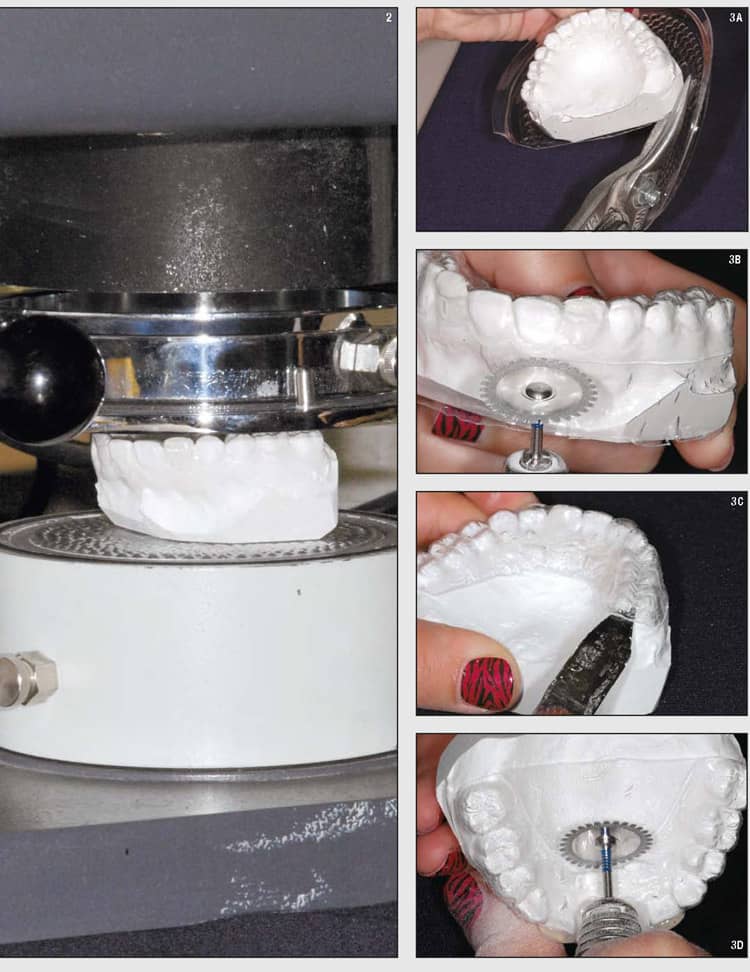
Figure 2: The cast is positioned in the thermoforming machine and covered with material. Figure 3: The margins are trimmed with scissors (A) then with a diamond disc (B). The palatal area is trimmed the same way (C, D).
Patient cooperation is critical. Patients with a history of noncompliance with requests for elastics and oral hygiene tend to continue this lack of cooperation with finishers. This can result in the same problems that we see in patients who don’t wear retainers full-time.
Beware of unrealistic expectations. Many times in attempting to finish a patient’s treatment, we may think, “I can complete that tooth movement with a finisher.” My experience over several years has prompted me to stay longer with brackets, bands, and archwires—and finish with less dependence on finishers.
Another issue is occlusal instability. Finishers do not permit complete occlusal interdigitation. If the patient is not stabilized by Class I molars and cuspids and appropriate cusp-fossa interdigitation, these unstable occlusions can become more unstable and/or relapse when placed in finishers.



Figure 4: After it has been removed from the model, the finisher is trimmed one more time (A), polished (B), and has its edges smoothed (C).
Shells



Figure 5: The completed finisher is placed in the patient’s mouth (A-C).
Another new technology to aid in finishing is what we call “shells.” Patients with poor oral hygiene tend to develop infected, swollen, and distorted gingival tissue. When we remove the orthodontic appliances from these patients, the resulting impressions are distorted by the inflamed gingiva. As a result, the finishers or retainers may be distorted or fit improperly. To solve this problem, we make impressions, but instead of attempting a treatment or making retention appliances, we use .020-inch sheets of a material similar to that which we use for finishers—except we trim these shells to the gingival margin. The result is appliances that hold the orthodontic correction, yet have no soft-tissue contact.
Patients like shells because they are almost invisible and comfortable. After the patient has worn the shells for 2 to 3 months, we can take new impressions that are not distorted by swollen, inflamed, or infected gingiva. These new impressions permit us to construct retainers or finishers that fit more accurately and thus function for the desired result.
Final Tips
One economic note bears mentioning. The extra steps of taking impressions, making models, and using pressure or suction machines and laboratory labor all add to our overhead cost of providing aesthetic, stable, and functional occlusions for our patients. It seems prudent to build these additional services into our fees at the beginning of treatment, rather than trying to justify additional fees at the end of treatment.
As with retainers, when placing the appliances, we do inform patients and parents that, while there are no additional fees for these appliances, there will be additional fees for losing or damaging the appliances. We stress to completely seat the appliance before biting down. If a patient bites finishers or shells to place them, the appliances will break, and such breakage requires new impressions, trimmed models, and skilled laboratory labor.
One final suggestion: When introducing any new technology or steps into your orthodontic practice, make sure to communicate clearly with patients and parents. In patient newsletters or letters to patients and parents, we always use a positive approach saying things such as, “To continue to offer you and your child the most innovative and ideal orthodontic treatment, we have chosen to add a proven, new technology termed, ‘finishers’ or ‘shells.’ ” We then list the advantages and the patient-cooperation requirements of these appliances.
I have found that adding this group of technological advances to our orthodontic treatment regimen has increased the satisfaction of my patients, parents, and orthodontic team.
Michael C. Alpern, DDS, MS, a member of Orthodontic Products’ editorial advisory board, is in private practice in Port Charlotte, Fla.










