by Moe Razavi, DDS, MSD
Combining appliance systems can shorten treatment time and lengthen appointment intervals

The recent increase in popularity of temporary anchorage devices (TADs) is due to the substantial treatment advantages they provide. It is now possible to move teeth in vectors previously unattainable without reciprocal movement on other teeth, while eliminating the need for patient compliance. Orthodontists can now move teeth in the anteroposterior and vertical directions with extreme predictability.
Miniscrew implants (MSIs) are a subset of TADs that can easily be incorporated into routine orthodontic treatment to enhance the efficiency of the overall treatment outcome and patient experience. They can provide a direct source of anchorage when they directly receive the reactive forces of a moving tooth or group of teeth.1
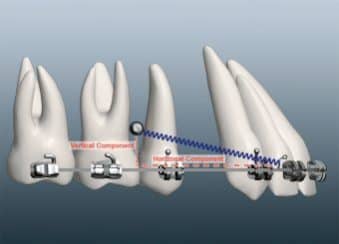
Figure 1: An interdental MSI loaded using coil springs. Note the vertical force vector as a result of direct loading of the MSI.

Figure 2: The vertical component of the force during space closure causes bowing of the archwire and lateral open bites.
Direct Anchorage

Figure 3: An MSI-stabilized TPA provides indirect anchorage during incisor retraction.
Commonly, you connect the segment of dentition you want to move to the MSI through an elastic chain module or a coil spring. MSIs are often placed interdentally in the buccal cortical bone. However, this anatomical site has complications such as limitations of interradicular bone, deviations in placement angle, impingement of the PDL space, and potential cementum contact, all of which increase the risk of premature MSI loosening and failure.2 Interdental MSIs can become obstacles in the path of moving teeth, especially when moving the entire arch in the AP direction. However, of greatest concern is that an MSI located interdentally and away from the archwire, when loaded with a Nitinol coil spring or a chain, introduces a force vector in the vertical dimension (Figure 1). This vertical force often causes undesirable side effects such as bowing in the archwire, leading to a lateral open bite and potential increased friction during space closure (Figure 2).
This side effect can be corrected during the final stages of treatment by using leveling archwires and interarch elastics to settle the occlusion. However, it leads to increased treatment time and requires patient compliance.
Indirect Anchorage
Alternatively, MSIs can be used as anchor devices indirectly by connecting a bar or a wire to the MSI and a stabilized tooth, which receives the reactive forces of tooth movement.1 The simplest indirect anchorage system is derived from a transpalatal bar connected to a TAD placed in the midsagittal regions. The palate provides one of the most suitable locations in the mouth for MSI placement, due to the abundance of dense cortical bone and the thick keratinized tissue, which ensure MSI stability and limit tissue irritation. Previous publications have described the benefits of placement of MSIs in the palate as well as the fabrication techniques of an appliance that combines an MSI with a transpalatal arch (TPA) and can be used with the Unitek™ TAD System.3-5
The main advantage of the indirect anchorage system provided by palatal MSI-TPA combinations is that they do not require any alterations in treatment mechanics. Clinicians can continue to use the same conventional orthodontic mechanics to which they are accustomed. Depending on the design of the MSI-TPA appliance, a palatal mini-implant can be used for en-masse retraction of anterior teeth (Figure 3), distalization of the entire maxillary arch, or protraction of the maxillary posterior segments.
The purpose of this article is to outline indirect palatal anchorage using the Unitek TAD system and the SmartClip™ Self-Ligating appliances in a nongrowing adolescent patient with a Class II, division 1 malocclusion and excessive overjet.
Treatment Progress
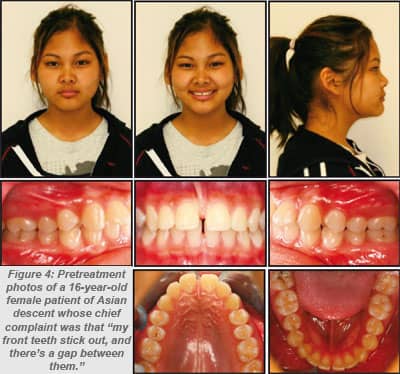
A 16-year-old female patient of Asian descent presented with the chief complaint of “my front teeth stick out, and there’s a gap between them” (Figures 4 and 5). The convex profile was due to acute nasolabial angle, resulting from the excessive proclination of the maxillary incisors. A Class II molar and canine occlusion was present due to mild mandibular retrognathia. Combined with the proclined maxillary incisors, this led to a 9-mm overjet and moderate overbite due to an exaggerated curve of Spee. There was mild spacing in both arches, with a large maxillary diastema and enlarged maxillary midline frenum.
The treatment objectives were to 1) close all spaces; 2) retract the maxillary incisors; 3) establish an ideal incisor relationship; 4) achieve acceptable posterior Class II molar occlusion; and 5) improve the acute nasolabial angle. The treatment plan included 1) extraction of maxillary first premolars; (2) full fixed appliances; 3) palatal MSI with TPA to stabilize maxillary molar position using indirect anchorage; 4) frenectomy of fibrous maxillary midline frenum; and 5) retention.


Figure 5: Pretreatment cephalogram and panoramic radiograph.
I used the SmartClip Self-Ligating appliance preadjusted with the MBT prescription. The brackets were direct bonded, and wires were sequenced to 0.019 x 0.025 stainless steel. My working archwires were enhanced with crimp-on hooks between the maxillary lateral incisors and canines to allow for en-masse retraction without the use of elastics or chain modules to close the spaces (Figure 6).

Figure 6: A crimp-on hook on a .019 x .025 stainless steel wire creates a posted wire for en-masse retraction.
The posted archwires were loaded with Nitinol closing coils. The coil springs provide control of the forces applied, and ensure continuous force application throughout space closure. Elimination of the elastics chain modules helped improve the overall oral hygiene. Recent studies have demonstrated a reduction of the total number of bacteria on teeth bonded with SLBs.6,7
I placed a 6-mm MSI at the level of the first premolars, 1 mm lateral to the midpalatal suture. The Unitek TAD System comes with a stainless steel healing O-Cap, which I placed on the MSI head before taking a pick-up impression. I used a working model to solder a 0.032 stainless steel wire to the O-Cap, and installed the TPA intraorally so that it stabilized the maxillary first molars (Figure 3). Adjustment appointments were made at intervals of 8 to 10 weeks. I activated the Nitinol coils to allow for incisor retraction and cut the distal extents of the wire for patient comfort (Figure 7).
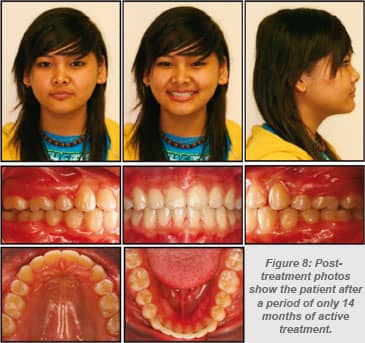
I removed the TPA and palatal MSI once all the extraction spaces were closed, and the detailing phase of the treatment was initiated. The patient was referred for a midline frenectomy. Prior to debond, I installed a fixed mandibular lingual retainer. Following debond, I used a removable maxillary clear vacuform retainer in the maxillary arch (Figure 8).

Figure 7: Distal extension of the wire at subsequent adjustment appointments.
Post-treatment cephalometric evaluation showed significant uprighting of the maxillary incisors. The maxillary molar position was stable, and the anchorage loss was less than 1 mm. A panoramic radiograph did not display evidence of root resorption or other pathologic problems. The final ABO Cast-Radiograph evaluation revealed a score of 10, well within the passing margin of the ABO.
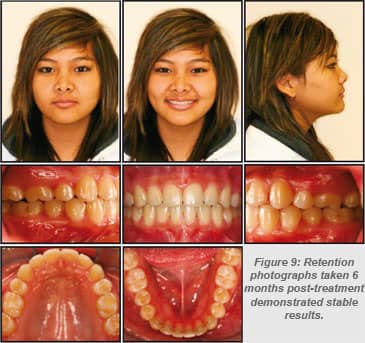
I saw the patient for a total of 11 appointments during the 14-month active treatment period. She was extremely satisfied with the final results, and further delighted in the shortened treatment duration given the fact that her commute to the orthodontic clinic was almost an hour each direction. A 6-month follow-up appointment demonstrated stable results (Figure 9).
Conclusion
Many interdental sites have proven effective for direct anchorage use of MSIs. However, for the clinician new to the world of MSI anchorage, the idea of placing a miniscrew between tooth roots may be intimidating. The palate, on the other hand, presents an environment that naturally limits tissue irritation and inflammation.8 Furthermore, MSIs located in the palate can predictably control both the position of maxillary dentition as well as the position of almost every tooth in the mouth. For orthodontists of all expertise levels with temporary anchors, the palate offers a safe haven for MSI placement.
A TPA attached to an MSI is a predictable means to control anchorage without altering treatment mechanics, as is often the case when MSIs are placed interdentally. Using this technique with the SmartClip Self-Ligating appliance allowed for a shorter treatment time than with conventional mechanics.
Today, patients have limited free time, and orthodontic visits at intervals of 4 to 6 weeks for 30 months are intrusive on their lives. Combining MSIs and SLBs offers the average orthodontist an attractive service to patients, since treatment time can be reduced without a compromise in the final treatment outcome.
Moe Razavi, DDS, MSD, has a private practice in Ottawa, Canada. He is an assistant clinical professor and director of the Skeletal Anchorage Clinic at Case Western Reserve University. He has worked on the craniofacial team at the Cleveland Clinic Foundation and as the orthodontist to the Cleveland Browns. He is a diplomate of the ABO. He has been an advocate for 3M Unitek since 2007, and has presented many lectures in the field of MSIs and SLBs. He can be reached at
References
- Papadopoulos MA, Tarawneh F. The use of miniscrew implants for temporary skeletal anchorage in orthodontics: A comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e6-e15.
- Baumgaertel S, Razavi MR, Hans MG. Mini-implant anchorage for the orthodontic practitioner. Am J Orthod Dentofacial Orthop. 2008;133:621-627.
- Razavi M. Temporary anchorage device techniques: Direct vs. indirect anchorage. Orthodontic Perspectives. 2008;14(1):6-8.
- Razavi M. Applications and benefits of fixed anchorage in the palate. Orthodontic Perspectives. 2009;16(2):15-17.
- Razavi M. Indirect anchorage using the palate: A unique applicaton of the Unitek Temporary Anchorage Device. Orthodontic Perspectives. 2010;17(2):6-9.
- Alves de Souza R, Borges de Araujo Magnani MB, Nouer F, et al. Periodontal and microbiologic evaluation of 2 methods of archwire ligation: Ligature wires and elastomeric rings. Am J Orthod Dentofacial Orthop. 2008;134:506-512.
- Pellegrini P, Sauerwein R, Finlayson T, et al. Plaque retention by self-ligating vs. elastomeric orthodontic brackets: Quantitative comparison of oral bacteria and detection with adenosine-triphosphate-driven bioluminescence. Am J Orthod Dentofacial Orthop. 2008;135:426-e1-426.e9.
- Kang S, Lee S, Ahn S, Heo M, Kim T. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop. 2007;131:S74-80.










