by Stephen Tracey, DDS, MS
Why these devices are not just an evolution but a revolution
“Come to the edge,” He said.
They said, “We are afraid.”
“Come to the edge,” He said.
They came. He pushed them … and they flew.
—Guillaume Apollinaire
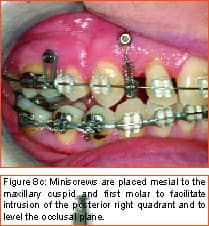
 |
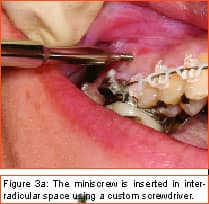
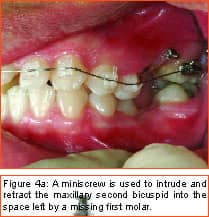
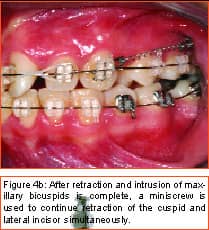
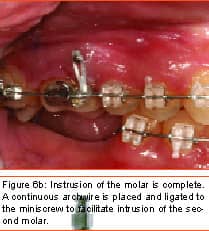
Philosopher, writer, art critic, and a man many consider the greatest French poet of the early 20th century, Guillaume Apollinaire beautifully described man’s primal fear of the unknown and the rewards that await those who are bold enough to “Come to the edge.” Throughout the history of our profession, bold men and women have continued to advance the art and science of orthodontics through their creativity, persistence, and willingness to evolve. In my career of nearly 2 decades, I have been privileged to witness some truly revolutionary advancements. Bonded brackets, nickel titanium archwires, noncompliance mechanics, self-ligating braces, cone-beam 3-D radiography, and sequential aligners have all made a tremendous impact on how we practice our craft. More recently, many practitioners have experienced the amazing capabilities of the soft-tissue laser in their efforts to be more efficient and produce final results that were previously unattainable. While all of these developments have had a tremendous impact on the way we practice, in my mind none will compare to the impact temporary anchorage devices (TADs), or more specifically, miniscrew implants (Figure 1, left) will have on our profession. Breaking Newton’s Third Law Until recently, orthodontists have been enslaved by Newton’s Third Law, which states that for every action there is an equal and opposite reaction. As a result, myriad intraoral and extraoral appliances have been used—with mixed results—in our efforts to minimize the movement of certain teeth while completing the desired movement of other teeth. Although the concept of temporary fixed anchorage was envisioned as early as 1945 by Gainsforth and Higley1, the first clinical report in the literature demonstrating the use of miniscrew anchorage appeared in 1983, when Creekmore and Eklund2 used a rather large vitalium bone screw placed in the anterior nasal spine to assist intrusion of maxillary incisors in a severe deep bite case. Unfortunately, the profession was not quite ready to “come to the edge” at that time, and the technique failed to gain immediate acceptance. However, beginning in the late 1990s, orthodontic researchers began to publish numerous case reports documenting the use of several different types of temporary anchorage devices. The bulk of this research came from Asia and Europe. Nearly 3 years ago I began to experiment with various forms of osseous anchorage, and I am now convinced that it is the next “new, new thing” in orthodontics. To Refer or Not to Refer Although initially we referred placement of miniscrews to our oral-surgeon colleagues, it became apparent very quickly that this not only made routine use prohibitively expensive and inconvenient for the patient, in all too many instances, it also resulted in the miniscrews being placed in positions not ideally suited for our purposes. So for some time now, we have been placing the miniscrews in our office and including it as part of routine orthodontic treatment. It is a simple, straightforward procedure that need not cause apprehension, either to the patient or the orthodontist placing the miniscrews. It is my strong opinion that placement of miniscrew-anchorage devices should be performed by the orthodontist. First, we have a much better understanding of root positions and orthodontic mechanics than any of our dental colleagues. Second, it is a very simple procedure that requires minimal anesthesia (in some cases, only topical anesthetic) and only a few minutes of time. Amazingly, there is virtually no pain involved either during the procedure or afterward. Third, in the event that a miniscrew becomes loose (and believe me, some will), it is much easier and more convenient for the orthodontist to replace it as needed. Incidentally, removing a miniscrew requires only topical anesthesia and a few seconds of time—and again, it is pain-free for the patient. Placement Sites Although miniscrews can be placed virtually anywhere there is sufficient bone and interradicular space, some sites seem to be more useful when our usual mechanics are used. These sites include areas where teeth are missing, between the roots of the second bicuspids and first molars— both on the buccal and lingual—and in the interradicular spaces both mesial and distal to the cuspids. Ideally, miniscrews should be placed in attached gingiva. At times this is not practical, but the orthodontist should know that when a miniscrew is placed in unattached gingiva, tissue overgrowth is likely. Although a number of articles have proposed the use of a variety of different surgical guides to determine acceptable miniscrew positions, we have found such guides to be of little benefit and impractical. Realistically, most orthodontists do not have the luxury of having a periapical x-ray machine in their offices. And because of the nature and limitations of intraoral radiography, even the slightest deviation of the x-ray beam due to variable cone position will result in radiographs that do not display accurate representations of the interradicular spaces. We have had a 100% success rate of miniscrew placement using nothing more than astute clinical observation and palpation combined with review of pre-orthodontic radiographs. Surgical Procedure After the proposed insertion site is determined, topical anesthetic is applied to the area and in the buccal vestibule if the miniscrew is to be placed buccally. Our topical anesthetic of choice is 20% lidocaine, 4% tetracaine, and 2% phenylephrine. We prefer this to other formulations for its ability to provide both profound anesthesia and vasoconstriction as a result of the action of the phenylephrine. This topical is left on for approximately 4 minutes. Although we have had some success placing miniscrews with topical anesthesia alone, it is our preference to combine topical anesthesia with local anesthesia to ensure a totally pain-free procedure. Also, by using lidocaine with epinephrine we gain additional hemostasis. Since we are making no attempt to anesthetize teeth, only a small amount of local anesthetic is injected into the adjacent vestibule and then directly into the gingiva where the miniscrew is to be placed. We then have the patient swish with chorhexidine gluconate rinse for 1 minute to decrease the likelihood of infection. While many of the miniscrews presently available are designed to be self-drilling, we have consistently been most successful drilling a small pilot hole with a slow-speed contra-angle handpiece prior to miniscrew placement (Figure 2, page 22). This pilot hole is meant only to provide a stable purchase point and facilitate accurate directional control when threading the miniscrew into the bone. Consequently, care should be taken to just perforate the cortical plate, at which time decreased resistance will be felt, signaling the operator to cease drilling. Attempts to create a pilot hole any deeper will result at best in a loose-fitting miniscrew, and at worst in the perforation of a root. Should irrigation be needed, we like to err on the safe side and use sterile saline expressed from a syringe, rather than using an air-water syringe and risking possible contamination from biofilm. The miniscrew is then placed into the driver (which in most cases resembles some form of a screwdriver) and then is carefully threaded into the bone (Figure 3, pages 22 and 24). Should significant resistance be encountered, one explanation could be engagement of a tooth root, in which case the miniscrew should be withdrawn slightly and redirected. While a variety of miniscrew sizes are presently available from a number of companies, a majority of the most common sites used are best served by the placement of a miniscrew that is 6 mm to 8 mm long with a diameter of about 1.4 mm to 1.6 mm. Although some practitioners advocate waiting approximately 2 weeks to load the miniscrew, we have had excellent success loading it immediately using forces ranging from 50 to 200 grams. Mechanics should be designed to direct forces applied to the miniscrew through it, avoiding lever arms that create excessive rotational moments. Applications Although the use of miniscrew anchorage is limited only by the orthodontist’s expertise, experience, and imagination, typical applications include the following: 1) Anchorage control in space closure: Whether closing space present from extracted or missing teeth (Figure 4, page 24), or created as a result of molar distalization (Figure 5, page 24), use of miniscrew anchorage provides uncompromising control. 2) Intrusion of hypererupted dentition: In the past, intrusion of significantly hypererupted posterior teeth was virtually impossible. The use of miniscrew anchorage allows trouble-free intrusion of these problematic teeth (Figure 6, left). 3) Extrusion of impacted cuspids: In many instances, the precarious position of an impacted cuspid can create an extremely challenging problem and limit our ability to safely and effectively bring it into the arch. Miniscrew anchorage allows for unusual force vectors that are otherwise unattainable (Figure 7, left). 4) Leveling the occlusal plane: Canted occlusal planes have traditionally been accepted, ignored, or—in worst-case scenarios—referred for correction with orthognathic surgery. Miniscrew anchorage can now be effectively used to correct asymmetries and canting of the occlusal plane (Figure 8, pages 26 and 28). Summary Could it be that orthodontics has finally found the “holy grail” we have all been searching for—simple, stable, uncompromising anchorage? I truly believe that miniscrew implants will prove to be a revolution in our profession. While initial acceptance may build slowly at first due to natural hesitations experienced by many orthodontists, ultimately I am confident it will become a routine, “bread-and-butter” procedure used by a majority of practitioners once they have had the opportunity to experience how simple miniscrew implants are to place, and how powerful they are to use. It is time to come to the edge … and fly! z Stephen Tracey, DDS, MS, is a Diplomate of the American Board of Orthodontics and a member of the AAO, the World Federation of Orthodontists, and the Academy of Laser Dentistry. He maintains a practice in Upland, Calif, and is an internationally recognized lecturer, with past presentations made in 15 countries on six continents. He can be reached at (909) 981-8789 or [email protected]. References 1. Gainsforth BL, Higley LB. A study of orthodontic anchorage possibilities in basal bone. Am J Orthod Oral Surg. 1945;31: 406–416. |