by BjÖrn Ludwig, DMD, MSD; Bettina Glasl, DMD, MSD; Thomas Lietz, DMD; Joerg Lisson, DDS, PhD; and S. Jay Bowman, DMD, MSD
A new North Star for orthodontics
Ancient mariners used the constellations and their individual component stars as landmarks from which to navigate, often in uncharted waters, as they discovered new horizons during their journeys. The advent of miniscrew anchorage provides a new reference, a kind of Polaris or “North Star,” that allows today’s orthodontist to plot courses of treatment that may have been previously unpredictable or even impossible with traditional mechanics.
In view of the plethora of publications, continuing education courses, and marketing materials available to our specialty on the subject of skeletal anchorage, it would seem that the use of miniscrews has become ubiquitous. The reality is much different. In actuality, very few orthodontists have yet to embrace miniscrew use in daily clinical practice. Those who have set sail into this unfamiliar territory have employed them sparingly, and many have elected to have someone else insert them for their patients. It is the authors’ intended purpose to encourage hesitant practitioners to come aboard and incorporate miniscrews on a more routine basis.
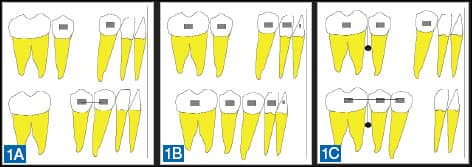 |
| Figures 1A–1C: Anchorage quality demonstrated by canine retraction mechanics. Expected results for a) minimum; b) medium (reciprocal); and c) maximum anchorage. |
Anchorage Concepts
In order to move an object, some type of anchorage or countersupport is required to stabilize a force applied to that object. In his Third Law, Sir Isaac Newton specified that every action has an equal and opposite reaction. If we are discussing support for orthodontic tooth movement, then forces that are applied between or across teeth will act on all of the dental units involved, perhaps resulting in unintended tooth movement of the so-called “anchor” teeth. The extent of this movement and also the countermovement depends upon the anchorage support derived from the individual teeth. In other words, dental anchorage is based on the number of teeth, the length of their roots, the root surface areas, and the structure of the supporting bone surrounding the teeth.
Anchorage quality in orthodontics can be divided into three categories: minimum anchorage, medium anchorage, and maximum anchorage. These three categories may be easily described with the example of conventional canine retraction after removal of a first premolar (Figure 1). If only the individual teeth involved in the mechanism provide support, you have minimal anchorage. Figure 1A demonstrates that a single premolar will not provide sufficient anchorage to retract the canine; rather, the premolar will likely be moved mesially, and there will be anchorage loss. Figure 1B shows two equal anchorage segments where action and reaction are comparable, and the result is medium anchorage and reciprocal tooth movement. In Figure 1C, the posterior group of teeth is secured and stabilized with a miniscrew (indirect anchorage). The canine can then be retracted without mesial movement of the posterior teeth as the reactive force is completely absorbed by the anchorage block. This is maximum anchorage.
Apart from the quality of the anchorage, the location of the anchorage support is also an important factor. A multitude of different anchorage devices have been employed throughout the first century of our specialty.
Methods of dental or desmodontal support have included the following:
- intraoral, intra-arch devices (such as the Nance holding arch, transpalatal arch, lingual arch, and lip bumper);
- modification of fixed appliances (buccal root torque to move roots into the cortical plate, blocking groups of teeth together, tip-backs or “setting anchorage,” uprighting springs and auxiliaries); and
- interarch mechanics (Class II or III elastics, fixed functional appliances).
Extraoral support has been provided by headgear and face masks.
The tools of skeletal anchorage support include implants, on-plants, and miniscrews.
This article describes anchorage only within bony structures; therefore, the terms “skeletal” and “cortical” anchorage are used interchangeably.
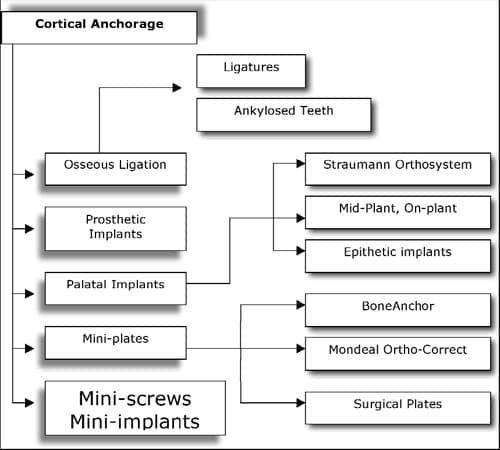 |
| Figure 2: The range of cortical anchorage options. |
History and Overview of Skeletal Anchorage
The era of skeletal anchorage began in 1945 when Gainsforth and Higley1 inserted screws into jawbone. Many experiments were unsuccessful, and the method had become virtually obsolete by the late 1970s. Starting again in 1980, various research groups (such as Creekmore and Eklund,2 Roberts et al,3-5 and Turley et al6,7) took up the subject once more. Creekmore and Eklund2 published the first clinically successful patient treatment case in which a metal post served as anchorage to intrude maxillary incisors and reduce an overbite.
There are now numerous options for cortical anchorage, ranging from the use of (artificial or pathologically) ankylosed teeth to miniplates (adapted from orthognathic surgery) and even prosthetic osseointegrated implants (Figure 2). Wehrbein and co-workers8-10 were the first to present an implant system specially designed for orthodontics (the Orthosystem from Straumann). Another example, the Midplant (HDC), was designed, like the Orthosystem, to be inserted into the palate. Both methods have been demonstrated to be safe and successful.
In recent years, the requirements for cortical anchorage techniques have been carefully defined in the literature.11-14 Under closer inspection, miniscrews appear to have the edge compared to other methods due to numerous advantages:
- biocompatibility;
- small size;
- simplicity of insertion and use;
- favorable primary stability;
- capacity for immediate loading;
- adequate resistance against orthodontic forces;
- ability to enhance typical orthodontic mechanics, often independent from patient cooperation;
- improved treatment effectiveness and efficiency;
- ease of removal; and
- cost-effectiveness.
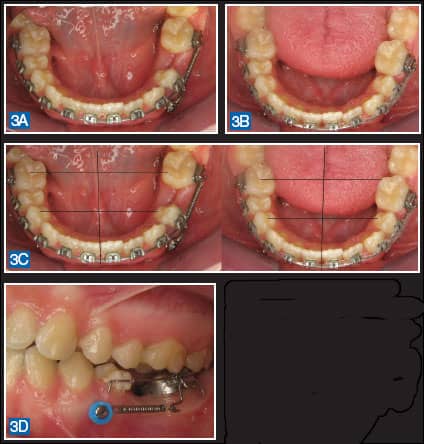 |
| Figures 3A–3D: Examples of miniscrew-supported mechanics for predictable unilateral space closure. Miniscrews prevented the typical reactive side effect of midline shift or anterior anchorage loss that would have occurred with traditional orthodontic mechanics. |
Miniscrew Properties
All types of skeletal anchorage (including miniscrews) are, by definition, implants. It is important, however, to differentiate miniscrews from typical dental implants.
More than 30 different terms for skeletal temporary anchorage screws are in use in the international literature. The most common of these are mini-implant, mini-pin, miniscrew, or TAD (temporary anchorage device). The term “miniscrew” appears to provide the most accurate (and most palatable) description of these “miniature screws,” especially when discussing their use with prospective patients (Figure 3). There are also more than 30 manufacturers of miniscrew systems (Figure 4), with the number of different screws offered per system ranging from two to 154. It can be an overwhelming and perplexing process to sort through all of these options and select those devices that are needed for daily practice. The following is an overview of the most important decision-making criteria for choosing a miniscrew system.
 |
| Figure 4: Eight examples of the more than 30 miniscrews that are currently available. From left to right: Ortho Easy from Forestadent, Aarhus from American Orthodontics, AbsoAnchor from Dentos, Dual Top from Jell Medical, LomasMondeal, Osas from Dewimed, Spider Screw from HDC, and tomas from Dentaurum. |
Materials
Miniscrews are typically fabricated from pure titanium or from an alloy of titanium with aluminum or vanadium. The safe biocompatibility of these materials when in direct contact with bone has been clearly proven in the literature.
Osseointegration
Branemark15 was the first to define the concept of osseointegration. He described it as “a direct functional and structural link between living bone tissue and the surface of a force-absorbing implant.”15-17 Several authors have indicated that there is no intention to anchor miniscrews by osseointegration; rather, primary retention is described as a “skeletal resistance block.”18,19 In the opinion of Cope20 and Bumann and co-workers,21 miniscrews are specifically anchored by mechanical stabilization and not by osseointegration. Since typical dental analogue implants and miniscrews are fabricated from the same materials, there appears to be nothing to preclude osseointegration, except the lack of surface coating and the smaller surface area of the miniscrew.
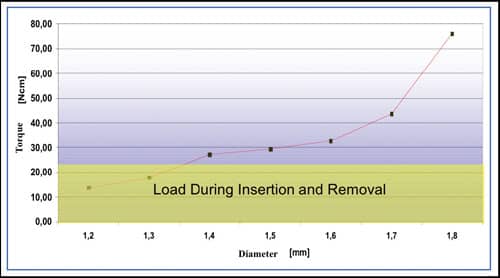 |
| Figure 5: Loads to miniscrews as determined by diameter. |
 |
| Figure 6: A radiograph demonstrating the range of available interradicular space for placement of a miniscrew. |
Miniscrew Diameters
The stability of a miniscrew in the bone depends primarily on its diameter, and not on its length (Figure 5).22-23 The diameter of available miniscrews varies between 1.2 mm and 2.3 mm. In this case, “diameter” is the outside diameter of the threads. For safe and secure primary mechanical stabilization, a minimum amount of bone is required around the shank of the miniscrew (Figure 6). Although there is no definitive answer as to the amount of bone required, it appears that from between 0.5 mm to 2 mm is necessary for stabilization to reduce premature loss. The amount of bone between the roots of teeth, therefore, defines the maximum diameter of screw that can be used in a particular site. In short, the total distance between roots should be at least 1 mm greater than the diameter of the chosen miniscrew to provide adequate bone support.
It is preferable to place miniscrews through attached mucosa. Not only is the insertion easier, but there is also less risk of tissue damage and subsequent tissue irritation or overgrowth of the implant. Publications by Poggio et al,24 Schnelle et al,25 and Costa et al26-27 provide some clues as to the vertical distance that is typically available between the cementoenamel junction (CEJ) and the mucogingival junction (MGJ). These investigations clearly show that the diameter of an interradicular miniscrew should not exceed 1.6 mm. An exception may be miniscrews inserted into the infrazygomatic ridge or on the lingual alveolus between the maxillary first molar and the second premolar. This, in fact, is the site with the widest interradicular space28 (Figure 7).
 |
| Figure 7: Larger-diameter (2-mm) miniscrews may be inserted between the maxillary first molars and second premolars to provide more stable anchorage support for molar distalization (without anchorage loss that can result from standard dental anchorage) for the Horseshoe Jet (a modification of the Distal Jet from AOA Laboratories, Racine, Wis). Since the roots of the second premolars are angled toward the buccal, they will bypass 8-mm miniscrews that are inserted at an angle to the cortical bone. This precludes the need to reposition miniscrews after the molars have been distalized (as is required when they are inserted into the buccal alveolus). The distal set-screw is then locked to convert the Horseshoe Jet to a miniscrew supported holding arch, and retraction of the remaining teeth is initiated. |
Miniscrew Lengths
The length of the various miniscrews on the market ranges from 5 mm to 14 mm. Typically, the length of the miniscrew refers only to the shaft or shank (the threaded section). As with the diameter, the selection of the length of a miniscrew is dependent upon the amount of bone available. Depending on the region, the total thickness of the alveolus is between 4 mm and 16 mm.29
The length of a screw, however, is of secondary importance when it comes to secure anchorage—the diameter is much more critical. Various investigations have shown that the thickness of the cortical plate plays the most important role in miniscrew stability.30-32 For example, FEM analyses have demonstrated that the typical orthodontic load is applied only in the region of the cortical bone.33,34
When selecting the length of a miniscrew, the depth of the gingiva must also be considered. The average depth of the gingiva is about 1.25 mm except in a few locations such as the retromolar region. The ratio between the length of the head (the part of the miniscrew outside the bone) and the length of the threaded shaft (the part of the screw inside the bone) should be at least 1:1. Consequently, Poggio et al24 recommended miniscrews lengths of 6 mm to 8 mm, and Costa26,27 suggested that miniscrews should be from 6 mm to 10 mm. On the basis of these investigations, it would appear that longer screws are unnecessary except in unusual circumstances. This has also been confirmed by numerous, anecdotal clinical experiences.
Color-coding of miniscrews for different lengths or diameters helps to facilitate the selection process. This color-coding is accomplished by an anodized surface coating (such as that used by Forestadent’s Ortho Easy). This oxide layer also appears to enhance retention of the miniscrew.35
 |
| Figures 8A and 8B: Height or profile difference for two clinical situations. |
Miniscrew Head Design
Some suppliers have a special head variation for every potential orthodontic application including:
- hook tops;
- ball-shaped heads;
- eyelets;
- simple slots;
- cross-shaped slots; and
- universal heads.
The screw head must be very small and compact (low profile) to ensure that the patient experiences minimal discomfort and tissue irritation (Figure 8). On the other hand, the head must also be large enough so that the coupling elements (such as coil springs, wire segments, auxiliaries, and elastic chains) can be easily and securely fastened to it (Figure 9).
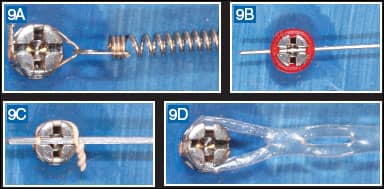 |
| Figures 9A–9D: For practical reasons, it may be advisable to use miniscrew systems that offer a single, universally applicable head design. It would seem feasible to connect all types of force elements (elastic threads, elastic chains, round wires, square wires, coil springs, auxiliaries, etc) to one ideal head design, facilitating the application of direct and/or indirect anchorage support to the same miniscrew design. |
Transgingival Portion
The transgingival portion, also known as the gingival neck, is a most important part of a miniscrew. Perforation of the gingiva occurs when a miniscrew is inserted. This provides a potential access route for microorganisms, thereby posing a risk of perimucositis or peri-implantitis, one of the main causes of premature loss of miniscrews.36-37 During the immediate postoperative phase, the mucosa should adapt as closely as possible to the screw to seal the area.38 The most advantageous shape for that to occur appears to that of a cone, as this shape naturally results in a safe seal without a pressure zone. A cone-shaped transgingival collar appears to seal the mucosal perforation wound, much as a cork seals a bottle, and it may help to reduce bleeding. Some miniscrews feature no transgingival collar so that the screw resembles a pan-head screw. These types of miniscrews may result in a void between the screw and the soft tissue that could provide a site for plaque or debris accumulation.
Simplification of Inventory
It seems readily apparent that choosing a specific miniscrew that could be used for the majority of clinical applications would simplify the process of incorporating them into daily practice. Miniscrews with a head design featuring either some type of cross-slot or tube can be used for both direct and indirect anchorage mechanics. In addition, screws of 1.4 mm to 1.6 mm in diameter provide for adequate strength and sufficient primary stability (dependent upon available bone), and only upon occasion will larger-diameter screws be needed (for placement in the infrazygomatic ridge or lingual alveolus between the upper first molars and second premolars). Miniscrews 8 mm in lengths are suitable for the majority of applications; however, a few screws of 6 mm and 10 mm length could be kept on hand for specific locations.28 These guidelines should help you to streamline your selection process and maintain a cost-effective inventory.
Conclusions
Although the application of skeletal anchorage concepts to traditional orthodontic mechanics has opened new vistas of treatment predictability, effectiveness, and efficiency, universal adoption of miniscrews throughout our specialty will endure some growing pains. Although miniscrews are not vital for the majority of patient care, they can certainly improve many aspects of specific treatment mechanics and help to reduce reliance upon patient compliance.
It has been more than 75 years since the concept of skeletal anchorage was conceived, but now the imagination and inventiveness of today’s orthodontists are making its application feasible, safe, and reliable for daily clinical use. Certainly, significant due diligence and careful continuing education are a necessity prior to adopting miniscrew anchorage. Perhaps miniscrew anchorage will soon be seen as a new reference point or “North Star” on which a constellation of predictable orthodontic mechanics may be based.
BjÖrn Ludwig, DMD, MSD, is in private practice in Traben-Trarbach, Germany. He can be reached at
Bettina Glasl, DMD, MSD, is in private practice in Traben-Trarbach, Germany. She can be reached at
Thomas Lietz, DMD, is in private practice in Neulingen, Germany.
Joerg Lisson, DDS, PhD, is the head of the orthodontic department at the University of Homburg/Saar, Germany.
S. Jay Bowman, DMD, MSD, is in private practice in Portage, Mich. He can be reached at
References
- Gainsforth BL, Higley LB. A study of orthodontic anchorage possibility in basal bone. Am J Orthod Oral Surg. 1945;31:406-417.
- Creekmore TD, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod. 1983;17:266-269.
- Roberts WE, Smith RK, Zilberman Y, Mozsary PG, Smith RS. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86:95-111.
- Roberts WE, Marshall KJ, Mozsary PG. Rigid endosseous implant utilized as anchorage to protract molars and close an atrophic extraction site. Angle Orthod. 1990;60:135-152.
- Roberts WE, Nelson CL, Goodacre CJ. Rigid implant anchorage to close a mandibular first molar extraction site. J Clin Orthod. 1994;28:693-704.
- Turley PK, Kean C, Schur J, et al. Orthodontic force application to titanium endosseous implants. Angle Orthod. 1988;58:151-162.
- Turley PK, Shapiro PA, Moffett BC. The loading of bioglass-coated aluminium oxide implants to produce sutural expansion of the maxillary complex in the pigtail monkey (Macaca nemestrina). Arch Oral Biol. 1980;25:459-469.
- Wehrbein H, Glatzmaier J, Mundwiller U, Diedrich P. The Orthosystem-a new implant system for orthodontic anchorage in the palate. J Orofac Orthop. 1996;57:142-153.
- Wehrbein H, Glatzmaier J, Yildirim M. Orthodontic anchorage capacity of short titanium screw implants in the maxilla. An experimental study in the dog. Clin Oral Implants Res. 1997;8:131-141.
- Glatzmaier J, Wehrbein H, Diedrich P. [The development of a resorbable implant system for orthodontic anchorage. The BIOS implant system. Bioresorbable implant anchor for orthodontic systems]. Fortschr Kieferorthop. 1995;56:175-181.
- Hobkirk J, Watson RM, Searson L. Introducing Dental Implants. Edinburgh: Churchill Livingstone, 2003.
- Ismail SF, Johal AS. The role of implants in orthodontics. J Orthod. 2002;29(3):239-245.
- Kappert H. Titan als Werkstoff fÜr die zahnÄrztliche Prothetik und Implantologie. Deutsch ZahnÄrztl Z. 1994;49(8):573-583.
- Listgarten MA, Buser D, Steinemann SG, Donath K, Lang NP, Weber HP. Light and transmission electron microscopy of the intact interfaces between non-submerged titanium-coated epoxy resin implants and bone or gingiva. J Dent Res. 1992;71(2):364-371.
- Branemark PI, Breine U, Adell R, Hansson BO, LindstrÖm J, Ohlson A. Intra-osseous anchorage of dental prosthesis. I. Experimental Studies. Scand J Plast Reconstr Surg. 1969;3:81-100.
- Albrektsson T, Branemark PI, Hansson HA, Lindstrom J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155-170.
- Branemark PI, Zarb GA, Albrektsson T: Tissue-Integrated Prostheses. Chicago: Quintessence Publ Co, 1985
- Costa A. Orthodontic anchoraging implants. Mondo orthodontico. 2001;26(6):481-488.
- Maino BG, Mura P, Bednar J. Miniscrew Implants: The Spider Screw Anchorage System. Semin Orthod. 2005;11(1):40-46.
- Cope JB. Temporary anchorage devices in orthodontics: A pardigm shift. Semin Orthod. 2005;11(1):3-9.
- Bumann A, Wiemer K, Mah J. tomas – eine praxisgerechte LÖsung zur temporÄren kieferorthopÄdischen Verankerung. Kieferorthop. 2006;20(3):223-232.
- Poggio PM, Incorvati C, Velo S, Carano A. “Safe zones”: a guide for miniscrew positioning in the maxillary and mandibular arch. Angle Orthod. 2006;76(2):191-197.
- Schnelle MA, Beck FM, Jaynes RM, Huja SS. A radiographic evaluation of the availability of bone for placement of miniscrews. Angle Orthod. 2004;74(6):832-837.
- Costa A, Pasta G, Bergamaschi G. Intraoral hard and soft tissue depths for temprary anchorage devices. Semin Orthod. 2005;11(1):10-15.
- Costa A. Bone and soft tissue depths. In: Cope JB, Ed. OrthoTADs The clinical guide and atlas. Dallas: Under Dog Media LP; 2006.
- Cheng SJ, Tseng IY, Lee JJ, Kok SH. A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorage. Int J Oral Maxillofac Implants. 2004;19(1):100-106.
- Miyawaki S, Koyama I, Inoue M, Mishima K, Sugahara T, Takano-Yamamoto T. Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2003;124(4):373-378.
- Bowman SJ. Thinking Outside the Box with miniscrews, In: McNamara JA, Jr, ed. Microimplants as Temporary Orthodontic Anchorage. Ann Arbor, Mich: Craniofacial Growth Series; 2008(45).
- Costa A, Pasta G, Bergamaschi G. Intraoral hard and soft tissue depths for temprary anchorage devices. Semin Orthod. 2005;11(1):10-15.
- Miyamoto I, Tsuboi Y, Wada E, Suwa H, Iizuka T. Influence of cortical bone thickness and implant length on implant stability at the time of surgery – clinical, prospective, biomechanical, and imaging study. Bone. 2005;37(6):776-780.
- Nkenke E, Hahn M, Weinzierl K, Radespiel-Troger M, Neukam FW, Engelke K. Implant stability and histomorphometry: a correlation study in human cadavers using stepped cylinder implants. Clin Oral Implants Res. 2003;14(5):601-609.
- Wilmes B, Olthoff G, Bortoluzzi V, Drescher D. Impact of bone quality on primary stability of orthodontic mini-implants. Paper presented at: EOS Congress; July 4-8, 2006; Vienna, Austria.
- Abdelgader I, Keilig L, Bourauel C, JÄger A. Numerical and experimental investigation of different types of mini implants for orthodontic anchorage. World J Orthod. 2005;6(Supplement):314-315.
- Dalstra M, Cattaneo PM, Melsen B. Load transfer of miniscrews for orthodontic anchorage. Orthodontics. 2004;1(1):53 – 62.
- Suba C, Kovacs K, Kiss G, et al. Surface analysis of interaction between titan implants treated with anod oxidation and the human organism. Orv Hetil. 2004;145(41):2085-2091.
- Park HS, Jeong SH, Kwon OW. Factors affecting the clinical success of screw implants used as orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006;130(1):18-25.
- PrÄger T, Holtgrave EA. Primary stability of self-drilling and conventional screw implants for orthodontic anchorage. J Dent Res. 2003;82(special issue B):B-301 2319.
- Mah J, Bergstrand F. Temporary anchorage devices: a status report. J Clin Orthod. 2005;39(3):132-136; discussion 136; quiz 153.