In my practice, 40% to 50% of cases are adults who bring particular challenges to the consultation. Such challenges include periodontal issues, mutilated or worn teeth, occlusal discrepancies, and, quite often, missing teeth. The majority of adult patients who present with missing teeth had orthodontic treatment 25+ years prior, which involved four bicuspid extractions. All too often, the scenario is the same. The patient has a Class l occlusion with tipped-in canines and buccal segments, a dished-in profile that has contributed to poor facial aging as well as loss of arch length, resulting in crowding. Usually, what these patients want addressed does not match what orthodontists can accomplish without surgery. The following case is such an example.
Diagnosis
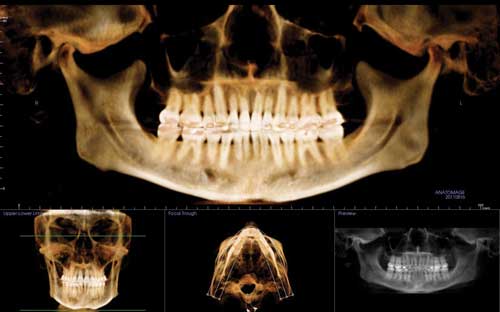
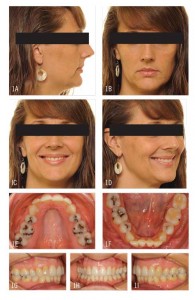
When this 40-year-old patient presented, she stated her chief complaint as, “I’ve lost my smile and hope you can help me get it back.” She had had four-bicuspid-extraction treatment 25 years earlier and was experiencing less than ideal facial aging because of lack of upper midface support. Like most patients with a similar history, she exhibited a Class I molar and canine relationship with moderate lower anterior crowding and dumped-in canines and buccal segments with narrow arches. Her profile had suffered greatly as she aged, and she now exhibited a concave profile with a general lack of midface support with reduced vermillion display. She was seeking orthodontic retreatment, hoping to recapture a more youthful appearance (Figure 1).
The majority of my adult cases require relatively straightforward treatment of 12 months or fewer to align the occlusion, broaden the arch in the buccal segments, and enhance the smile arc; but this approach, for this patient, would have improved her profile only minimally and would not accomplish what she desired. For her case, then, I presented two treatment options. Option 1 was the straightforward approach just mentioned. Option 2 would require at least 24 months of treatment time, but would enhance her face, particularly the midface and upper lip, by opening the closed extraction sites, then either placing implants or using temporary anchorage devices (TADs) to protract the posterior teeth. The patient chose the second option, then to finish treatment, the use of TADs to close the newly opened spaces by moving the posterior teeth forward.
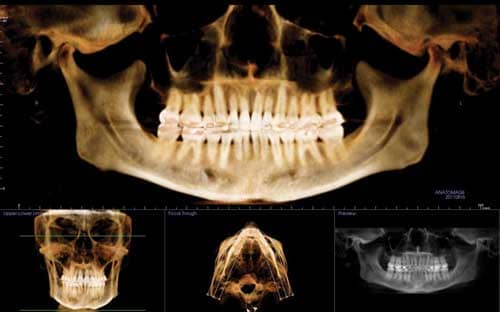
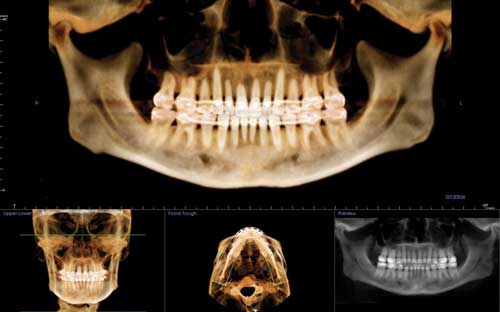
It was also noted during the pretreatment examination that the patient had slight, generalized bone loss with shortened roots on the upper and lower arches 2-2, more than likely from prior orthodontics. As we discussed the risks and benefits f treatment, I made certain she understood that further orthodontic treatment could possibly cause additional root shortening and bone loss. A cross-sectional study of the CT scan showed that the upper right cuspid exhibited thin buccal bone support and if gingival stripping occurred during treatment, a soft-tissue gingival graft would be indicated.
Treatment Planning
The treatment plan was to open space where the bicuspids had previously been extracted, then use Ormco’s VectorTAS™, a temporary anchorage device or TAD, to protract the posterior teeth. The estimated treatment time was 24 months, using Ormco’s Damon™ Q passive self-ligating brackets (Damon™ Clear upper 3-3). I find that the decreased friction of this passive self-ligating system keeps forces light and works beautifully in cases such as these where posterior arch development is key to a successful outcome.
Variable torque was employed on the upper and lower anteriors: low torque on the upper and lower arches 2-2 with standard torque on the upper cuspids and high torque on the lower cuspids.
After the closed extraction sites were open, two TADs would be placed anterior to the cuspids for anchorage and then the posterior segments would be protracted with medium-light nickel-titanium closing springs.
It would have been a disservice to my patient to open the closed extraction sites without controlling the torque of the anterior teeth. Because of the patient’s severe upper lip deficiency, the strategy was not only to broaden the transverse arch but also to position the upper anterior teeth as far forward as possible without compromising the buccal bone and roots of the anterior teeth.
Initial Bonding
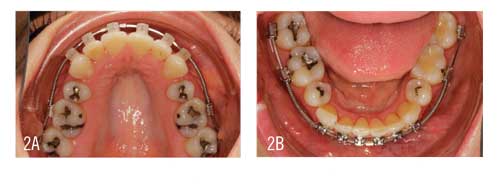
At the initial bonding, brackets were bonded on both arches 7-7 except on the 5s. A half-of-a-bracket width of coil spring was added to the upper teeth 6-3, bilaterally. At the second appointment, 6 weeks into treatment when the .018″ wire was engaged, a half-of-a-bracket width of coil spring was added to the lower teeth 6-3, bilaterally. The rationale for these protocols was to begin the space opening on the maxilla first in order to keep it ahead of the space opening on the mandible.
5 Months: Arch Broadening and Space Opening Exhibited
By 5 months into treatment, having moved through a progression of light, round, and smaller rectangular wires (.014″, .018″, and .014″ x .025″ Copper Ni-Ti), the upper archform had begun to broaden and the spaces were beginning to open with a slow half-of-a-bracket width of coil spring activation every 4 to 6 weeks. As planned, the space opening in the mandible was lagging behind that of the maxilla. Open coil spring activation would continue for another 12 months until the case was ready for TADs (Figure 2).
9 Months: Panograph/CT Scan/Repositions Performed
When the .018″ x .025″ Cu Ni-Ti wire has been engaged for 6 weeks, we routinely take photographs, a CT scan, and a panograph to evaluate the smile arc progression and root alignment relative to bracket placement, repositioning brackets as appropriate (Figure 3). I repositioned U2s and L2s and 3s. The reason for the photographs is to assess the buccal occlusion to assist in ensuring I don’t miss a repositioning opportunity.
18 Months: TADs Placed
Having placed the final stainless steel wires at the 16-month juncture (upper: .019″ x .025″ stainless steel; lower: .016″ x .025″ stainless steel), the case was ready for TADs 2 months later. I placed 6-mm TADs between the U2s and 3s and, with wire posts added mesial to the upper cuspids, ligated a .010″ ligature wire from the TADs to the cuspids. For maximum anchorage, the upper and lower anteriors were ligated 3-3 under the archwire and seven links of power chain were employed to tie back the U/L posts on the stainless steel wires to U/L6s.
The wires were clipped distal to the U/L 6s to allow the molars to slide forward. Note the 5s still have not been bonded. I decided it was better to wait to pick them up after space closure rather than stop the progress of treatment to do it then. With the TADs in place, the posterior teeth would begin to protract into the opened spaces (Figure 4).
Unfortunately, the incisors (both upper and lower) proclined slightly during space opening. I will detorque these teeth toward the end of treatment with TMA wires.
21 Months: TADs Removed
Removed the TADs, bonded the 5s, and changed to smaller dimension Cu Ni-Ti wires for 6 weeks, then placed TMA finishing wires (upper: .019″ x .025″; lower: .017″ x .025″) to correct the anterior torque, which took an additional 3 months.
Post-Treatment Analysis: 26 Months Total Treatment Time
This patient’s result was more than satisfactory (Figure 5). Her arches broadened appreciably, which diminished the buccal corridors. The uprighted buccal segments and appropriate incisor display and inclination offered increased lip and midface support, and along with the pleasing smile arc, did much to improve the youthfulness of her appearance.
As anticipated, the upper right cuspid lost attached gingival tissue, and the patient was referred to a periodontist for a gingival graft. Regrettably, I wasn’t able to fully open the bicuspid spaces. I opened as much space as possible without causing even more severe periodontal issues and keeping the patient in treatment two-and-a-half to 3 years.
These types of cases are very difficult to manage and can be tricky at best to finish well, so it’s imperative the coil spring activation to open the closed extraction sites be done with care and without overactivation. Overactivation results in flaring of the incisors and potential loss of control, which happened to a minimal extent in this case. Use of TMA wires at the end of treatment corrected the issue with lingual crown torque.
The result in this case would not have been possible were it not for the VectorTAS system. TADs are an important adjunct to orthodontics today that help reduce the need for placing implants or conducting invasive surgery in these types of cases.
At debond, after all of the contouring, smoothing, and polishing were done, I handed the patient a mirror and she began to cry. I was a little surprised, thinking that she didn’t like the result, and then she reached up with her hand and touched her upper lip and midface and said, “I have my smile back, and I am so happy.”
Labor-intensive, drawn-out treatments immediately become worthwhile when a patient’s face lights up with excitement and tears of joy. OP