by Keith Sherwood, DDS
A minimally invasive alternative to orthognathic surgery
The concept of implant-anchored orthodontics has been studied and written about for decades. Interest in the subject expanded after years of demonstrated success with titanium endosseus implants used for tooth restoration. In the past 6 years, the literature has seen a dramatic increase in reports on the placement of a variety of implant fixtures to assist in orthodontic treatment. Endosseus implants,1,2 onplants,3 miniscrews,4,5 and miniplates6,7 have all been used as skeletal anchors to support tooth movement.
Each implant system has strengths and weaknesses. In the future, it is unlikely that one type of implant will be used for every implant orthodontic application. Rather, different skeletal anchors will be indicated for treating distinct categories of orthodontic problems. Miniplates, for example, have been used with success for a variety of orthodontic anchorage needs, but have gained acceptance primarily as an alternative to orthognathic surgery for treating open bite.
Jenner and Fitzpatrick first reported on the use of a miniplate to retract mandibular molars in 1985.8 Since then, there have been numerous reports on the clinical application of miniplate anchorage. Titanium miniplates are attractive as an orthodontic implant anchor for a variety of reasons. They have been proven safe and effective as fixation plates for fractures and osteotomies in oral and maxillofacial surgery and orthopedics for more than 30 years. Their design allows the surgeon and orthodontist to avoid tooth roots when placing the plates and orthodontically moving teeth. They are adaptable to a variety of conditions. Finally, miniplates have been shown to be minimally invasive and safe as implant anchors.6,7,9,10
One of the more exciting applications of miniplate anchorage has been in the treatment of skeletal anterior open bites that would normally require orthognathic surgery. The use of miniplates on the maxillary strut7 or the buccal cortex of the mandible6 to assist in orthodontically closing open bites by intruding molars has been reported with increasing frequency. With more patients rejecting orthognathic surgery, miniplate-assisted orthodontic correction of open bite is an appealing alternative for patients and orthodontists.
 |
 |
 |
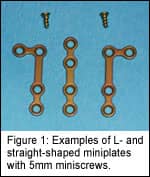
Most commercially available titanium miniplates used in orthognathic surgery are suitable for orthodontic anchorage. Figure 1 shows miniplates that come in a variety of shapes and sizes. The surgeon must have an assortment of lengths and shapes to meet the needs of the patient and the treatment plan designed by the orthodontist. As seen in Figure 2, the miniplate must be long enough to clear the roots of the teeth to be intruded and allow the last loop on the plate to project transmucosally into the buccal vestibule. The orthodontist uses this last loop on the miniplate to attach an elastic thread or other device to the bands or brackets on posterior teeth. For treating open bite, the posterior teeth are intruded, allowing auto-rotation of the mandible and closure of the anterior open bite.
A Burstone11 or similar cephalometric analysis should be done during pretreatment to determine if the open bite originates in the maxilla or the mandible. It has been shown that posterior vertical dentoalveolar excess is frequently the etiology of skeletal anterior open bite in adults.12 As a result, the maxillary strut is often the location of choice when planning miniplate placement. Orthodontic treatment usually precedes surgery by 4–8 weeks. Sectional archwires are usually placed 3-3 and 4-7 or 2-2 and 3-7, depending on the morphology of the open bite, and advanced to rectangular wires. It is critical that a continuous archwire not be placed in the arch where molar intrusion is planned, or the incisors will be extruded. Extrusion of incisors has been shown to be unstable, especially in adult patients.13 A trans-palatal appliance (TPA) or lingual arch must be placed prior to intrusion mechanics to prevent buccal tipping of molars. If a TPA is used, it must have palatal clearance equal to the expected molar intrusion.
At the time of surgery, the orthodontist will communicate to the surgeon how far apical to the molar roots the miniplate screws should be placed. The degree of open bite will determine how much intrusion is necessary and how much clearance is needed from the root apices. There is a 1:2 ratio between the amount of molar intrusion and the closure of the open bite. An intrusion of 4 mm, for example, will close an 8-mm open bite. The orthodontist should also describe to the surgeon where the miniplate should be placed in the sagittal plane. The miniplate loop emerging into the vestibule should be positioned adjacent to the tooth or teeth that need to be intruded the most.
The surgery is done with local anesthesia alone or with light sedation. A 1- to 2-cm incision in the mucobuccal fold to expose the cortical bone of the maxilla or mandible is required. An L-, Y-, or straight-shaped plate can be placed in the maxilla, while an L- or T-shaped plate will suffice for the mandible. The plate is contoured to the bone for stability. The emerging loop should be easily accessible for the orthodontist and will need adequate clearance from the molar band to allow intrusion. Two 1.5- to 2-mm-diameter miniscrews, each 5 mm long, are sufficient to fix the plate. The wounds are closed around the emerging miniplate loop. In our protocol, postoperative patients are placed on antibiotics for one week and allowed to heal for eight weeks before initiating intrusion mechanics.
An elastic thread or coil can be used to intrude the posterior segments (Figure 3). Although forces are difficult to measure in this area, 25 grams per tooth being intruded is theoretically ideal. If you are intruding two bicuspids and a molar, for example, you will need at least 100 grams of force to intrude the segment. This may vary tremendously between patients because of differences in root length and diameter. We have found that an elastic thread needs to be tied quite firmly to initiate intrusion with multiple teeth. After the first month, intrusion proceeds at 0.5 to 1 mm per month. Intrusion may advance more quickly in adolescent patients. The end point for intrusion is closure of the open bite. At this time, the miniplate loop should be tied to the molar band with a ligature wire until the remainder of orthodontic treatment is complete. After debracketing, nighttime retention with a wraparound retainer or, preferably, a retainer with posterior bite-blocks, is recommended. The miniplate is removed in a simple 10-minute procedure after the patient is in retention.
Closure of a skeletal, anterior open bite is one of the more challenging malocclusions for the orthodontist to manage. Long-term (10-year) predictability of traditional orthodontic treatment, such as extrusion of incisors, is often poor because it can be unstable even in younger patients.13 Other orthodontic approaches may prove ineffective, unaesthetic, or impractical. As a result, orthognathic surgery has often been the treatment of choice, especially in adult patients.
Open bite closure by intrusion of posterior teeth off miniplate anchors seems to be an effective treatment alternative. Risks and morbidity are minimal, although good periodontal health is essential to prevent infection. Research supports its effectiveness in appropriate patients.6,7,14 Ten-year stability has yet to be determined, although our experience over 5 years has been excellent. It is thought that intruded teeth are more stable than extruded teeth, especially in the molar area.15 The forces of occlusion may be adequate to maintain the intrusion.
Justification for treatment-planning any type of implant anchorage for your patient is based on answering an important question: Will skeletal anchorage facilitate correction of a malocclusion that would be difficult or impossible to manage with standard orthodontic care? Intruding posterior teeth with miniplates to close anterior open bites clearly meets this criterion. However, miniplates can also be used to intrude supererupted teeth16 and to distalize mandibular molars.17,18 In response to interest by the profession, miniplate companies have begun to design and market miniplate implants for use specifically as orthodontic anchors. These come with specially designed attachments on the exposed, intraoral end of the plate, which permit connection of the miniplate to an archwire. This potentially facilitates alternate uses beyond intrusion for the miniplate, including retraction, protraction, and eruption of teeth. Whether other types of implants are better suited to these alternate uses requires further research and clinical experience.
The orthodontist must act as “captain of the ship” in planning implant-anchored orthodontics. Determining the need for implant anchorage and the type of implant is an orthodontic decision. Discerning the ideal location for the implant requires active communication between the orthodontist and surgeon.
Although more needs to be done to refine clinical application and explore limitations, implant-based skeletal anchorage is increasingly assuming an important role in clinical orthodontics. Miniplates are an important part of this advance in technology. z
Keith Sherwood, DDS, is an orthodontist and a board-certified oral and maxillofacial surgeon. He was formally Co-Director of the orthodontic residency program at Nova Southeastern University College of Dental Medicine. He is currently in private practice both in orthodontics and oral and maxillofacial surgery in Chelmsford, Mass. He can be reached by email at [email protected].
References
1. Turley PK, Kean C, Schur J, Stefanac J, Hennes J, Poon LC. Orthodontic force application to titanium endosseous implants. Angle Orthod. 1988;58(2):151-62.
2. Roberts WE. Rate of mesial translation of mandibular molars using implant anchored mechanics. Angle Orthod. 1996; 66(5):331-337.
3. Block MS, Hoffman DR. A new device for absolute anchorage for orthodontics. Am J Orthod Dentofacial Orthop. 1995;107:251-258.
4. Liou EJ, Pai BC, Lin JC. Do miniscrews remain stationary under orthodontic forces? Am J Orthod Dentofacial Orthop. 2004;126(1):42-47.
5. Carano A, Velo S, Incorvati C, Poggio P. Clinical applications of the mini-screw-anchorage-system (MAS) in the maxillary alveolar bone. Prog Orthod. 2004;5(2):212-35.
6. Umemori M, Sugawara J, Mitani H, Kamamura H. Skeletal anchorage for open bite correction. Am J Orthod. 1999;115:166-174.
7. Sherwood KH, Burch JG, Thompson WJ. Closing anterior open bites by intrusion of molars using titanium miniplate anchorage. Am J Orthod Dentofacial Orthop. 2002;122:593-600.
8. Jenner JD, Fitzpatrick BN. Skeletal anchorage using bone bone plates. Aust Orthod J. 1985;9:231-233.
9. Daimaruya T, Nagasaka H, Umemori M, Sugawa J, Mitani H. The influences of molar intrusion on the inferior alveolar neurovascular bundle and root using the skeletal anchorage system in dogs. Angle Orthod. 2001;71(1):60-70.
10. Sugawa J, Baik UB, Umemori M, Takahashi I, Nagasaka H, Kawamura H, Mitani H. Treatment and posttreatment dentoalveolar changes following intrusion of mandibular molars with application of a skeletal anchorage system for open bite correction. Int J Adult Orthod Orthognath Surg. 2002;17(4):243-53.
11. Burstone CJ, James RB, Legan H, Murphy GA, Norton LA. Cephalometrics for Orthognathic Surgery. J Oral Surgery. 1978;36:269-77.
12. Frost D, Fonseca RJ, Turvey TA, Hall DJ. Cephalometric diagnosis and surgical-orthodontic correction of apertognathia. Am J Orthod. 1980;78(6):657-659.
13. Lopez-Galvito G, Wallen TR, Little RM, Joondeph DR. Anterior open bite malocclusion: Am J Orthod. 1985; 87(3):175-185.
14. Ervardi N, Keles A, Nanda R. The use of skeletal anchorage in open bite treatment: a cephalometric evaluation. Angle Orthod. 2004;74(3):381-90.
15. Reitan K, Rygh P. Biomechanical principles and reactions. In: Graber and Vanarsdall, editors. Orthodontics: current principles and techniques. 2nd ed. St. Louis:Mosby;1994:168-9.
16. Sherwood KH, Burch JG, Thompson W. Intrusion of supererupted molars with titanium miniplate anchorage. Angle Orthod. 2003;73(5):597-601.
17. Keles A, Everdi N, Sezen S. Bodily distalization of molars with absolute anchorage. Angle Orthod. 2003;73(4):471-82.
18. Sugawara J, Daimaruya T, Umemori M, Nagasaka H, Takahashi I, Kawamura H, Mitani H. Distal movement of mandibular molars in adult patients with the skeletal anchorage system. Am J Orthod. 2004;125(2):130-138.










