by Kelly Murray
How to turn the worst patient into the best patient

I love Johnny’s response: “No, but I did yesterday.” And I think, “Here’s another yuck-mouth patient who uses the wrong end of the toothbrush.” Thank goodness for masks, because the bad breath can take out the faintest of hearts. Then he opens, and I look inside and am horrified that there is so much plaque that the brackets are completely covered. Decalcification has set in. Or even worse, the gum tissue has grown over the brackets. So I pull up my mask and make sure the safety glasses are secure before going in.
Clean Teeth Move Faster
I always tell patients that good oral hygiene is essential when straightening teeth. The body’s process of breaking down bone and reforming bone is a fantastic function that happens at its own rate. This process can happen much more efficiently if the mouth is free and clear of debris.
It is our job as assistants to chart poor oral hygiene, inform the patient’s parents and the orthodontist, and then instruct and inspire the patient to keep his teeth clean. There is a fine balance and an art to turning a poor brusher into a stellar one. This can be done with a positive attitude and a lot of praise. Yes, I said praise.
You Gotta Believe
The first step to creating an awesome brusher is to believe the patient can and will follow the instructions and then keep it going. If we treat the patient as if he were the best brusher in the world, then we can help him and inspire him to make it happen. We as assistants see these patients every 3 to 4 weeks. We have a golden opportunity to strengthen their self-esteem and turn a negative action into a positive experience. It is not our job to berate or belittle a patient with a good amount of plaque on his teeth.
If we happen to come across as too harsh to the patient, all our good intentions are lost and the patient leaves the office feeling terrible and not wanting to ever see us or a toothbrush again. This can happen. Be very careful with teenage patients’ feelings. Choose your words cautiously, and always remember the Golden Rule. How would you like to be treated in this delicate situation?
Three Positives, One Negative
The second step to creating a better brusher is to find three positive things to say before mentioning the brushing issues. If the patient is a boy, I start looking for nice hair or new shoes, and I observe his attitude. I also make notes each time I see the patient so I can ask follow-up questions from his last visit. This is so important in building a trusting relationship and also in building up an emotional bank account. We must always make more emotional deposits than withdrawals. We never know the status of each patient’s emotional bank account, so it is always safer to start off by making kind comments to make the patient feel better.
I follow the “three positives to one negative” rule: I find three great things to say first. Then I take a look inside the mouth and start looking for something positive to point out. Even if I see only one tooth that looks brushed, I make a big deal about how great it looks. Then I send the patient to the sink to brush the rest of his teeth to make them look like the great brushed tooth. The patient is beaming, and I have gotten the point across with no battles, tears, or angry parents.
Pampering Parents
We need to avoid angry parents at all costs. All parents think their kids are perfect. Who is this mean person making their angel cry? We all know how fast we will see the inside of our orthodontist’s office, and that can almost never be good. So I watch my words and delivery carefully.
It is a professional thing to bring the parents to the chair and inform them of the situation. Remember to start the conversation in a positive way. “Hi, Mrs Smith. How are you today? I have the absolute pleasure of working with your brilliant, funny, sweet son or daughter.” At this point, I have accomplished two things. I have complimented the parents, and I have pointed out some of the patient’s strengths. I have made deposits into the emotional bank account.
The next thing I go into is how important brushing is in getting the teeth straight. I educate and instruct. I use pictures and models. I also make sure I cover all the learning types: auditory, visual, and tactile. We give a hygiene scorecard report every visit. A patient’s brushing is graded twice: once when he first sits in the chair, and then again after he brushes. We grade on an A to F scale, and if the grade is a C or lower, we diagram on the scorecard spots that the patient is missing and then show the patient these spots in the mirror.
Show, Don’t Tell
I show the patient posters and graphic pamphlets of really severe cases of periodontal disease, and tell him that this could happen to him if he is not careful. I also show him pictures of decalcification and explain in detail what it is and what causes it. I use a model with braces to teach brushing and flossing. I take the tip of the scaler and gently slide it up into the patient’s gum tissue. I have him watch this in the mirror, and I show him how food can get trapped in this pocket. I show him that the tip of the scaler should not disappear under the gums. I take the scaler and scrape some plaque off his teeth and ask him if he would like to eat it on a cracker.
I would love to have a microscope in the office. I would take the plaque, put it on a slide, and have the patient watch the bacteria moving around. Then I would tell him that these little bugs are living on his teeth and leaving their waste products on his teeth. The fact that the waste products from the bacteria are what cause decalcification, and that it acid-etches the teeth, is usually a shock to patients and their parents.
To Pick or Not to Pick
I have seen good results and bad results with water picks. The bad things that can happen are abscesses. If the patient is a poor brusher and flosser and he water picks instead, the water forces debris under the bands and traps it there, causing an abscess. We then have to remove the bands and remove the debris. Two weeks later we evaluate the patient for separators, then schedule for the bands to be replaced. This slows the treatment time down and causes the patient unnecessary pain and discouragement.
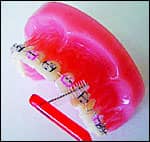
I think the best floss to use with braces is thick, furry floss. It has a stiff end that can be threaded under the wire and a thick, furry end that can be pulled through to get the plaque trapped between the teeth and the back bands. I show patients how to floss on a model, and then I show them how to floss inside their own mouths. I then have patients floss the model and floss inside their mouths.
I always demonstrate the techniques in front of the patient’s parents. If the parents are not with the child, I call the parents on the cell phone and ask them to come and see me. The best thing to do if you cannot get a parent to come in and see you is to document on the chart that the patient has poor oral hygiene, that tooth-brushing instructions were given, and that the parents were contacted. Documenting this covers the instance when the braces get removed and there are white spots present that the parents get upset about. All I have to do is show the parents the documentation of all the times oral-hygiene instructions were given and the parents were contacted.
A Brush With Greatness
Patients always ask which type of toothbrush is the best, and my response is always that it is the one that the patient will use. I have seen positive and negative results from electric and regular toothbrushes. It all comes back to time and technique. I really stress the flossing. I recommend that the patient flosses at least three times per day, and then I am assured that he will floss at least once. Every time I need to remove archwires for bends or to change the size of the wires, I encourage the patient to brush and floss. That way, I know for sure that he or she flosses at least every 4 weeks. I recommend a fluoride rinse. The rinse does two things: It makes the teeth slick so that plaque is less likely to stick, and it heals some of the minor decalcification scars on the teeth to stop the beginning of decay.
The Last Resort
When we get patients with severe gum-tissue swelling and bloody gums, we remove their wires, give them brushing instructions, and recommend warm, saltwater rinses and a fluoride rinse. We also show them all the visual aids. I follow up a few days later to see how the brushing and flossing is going, and to give encouragement and praise. We also recommend a cleaning and checkup with their general dentists if it has been more than 6 months since they saw them. We see patients back in 2 weeks to check the gum tissue and evaluate if the wires can be replaced. Usually their gums look really healthy, so we replace the wires and tooth movement begins again. The fact that tooth movement stops until they can get their gum tissue healthy is a huge motivator to get patients to keep their teeth clean.
I think the most important things to remember are: 1) Praise and motivate the patient. 2) Build a great, trusting relationship with the patient. 3) Document everything in red so it can be easily seen. 4) Have excellent communication with the patient’s parents, and keep them informed of the progress of the patient’s treatment and hygiene. 5) Teach excellent hygiene technique.
If you do all these things, just watch: Your practice will turn those patients with scarily bad oral hygiene into spectacular brushers.
Kelly Murray has been working in orthodontics for 16 years and is currently an orthodontic assistant for David Vaughn Bates, DDS, and Mark F. Maxwell, DDS, MS, in Newport Beach, Calif. She can be reached at (949) 640-0203.









