by Flavio Uribe, DDS, MDentSc; Aditya Chhibber, BDS, MDS; and Carlos Villegas, DDS
Eliminating presurgical orthodontics can decrease treatment time in adult patients with severe dentofacial deformity

Figure 1A: Pretreatment extraoral images show the patient’s combination of a retrognathic maxilla and prognathic mandible.

Figure 1B: Pretreatment intraoral images detail the patient’s full-cusp Class III molar and canine relation bilaterally, with a bilateral posterior and anterior crossbite. She also presented with 4 mm of reverse overjet with 50% deep bite and 4 mm of crowding in the upper and 6 mm of crowding in the lower arch, respectively.
The success of orthodontic treatment may generally be evaluated by the final result of treatment, the efficiency of treatment, and the stability of the treatment results. When evaluating efficiency, overall treatment time is one of the critical factors to be evaluated. Studies by O’Brien et al1 showed that children undergoing two phases of orthodontic treatment for the Class II malocclusion had no significant advantage over those who had one phase of treatment, lending credibility to the idea that one-phase treatment may be better than two-phase treatment, since the former can achieve similar outcomes in much less time.
Orthodontic treatment in adults with severe dentofacial deformity usually involves orthognathic surgery to correct the underlying skeletal discrepancy. The combined treatment time of orthodontics and orthognathic surgery is usually lengthy. The standard procedure with these patients involves three phases of treatment: a presurgical phase, surgery, and a postsurgical orthodontics phase. The main objective of the presurgical phase is to decompensate the upper and lower arches to achieve proper axial inclinations of the incisors, leading to a transitory detriment of facial aesthetics. The surgical procedure corrects the underlying basal bone relationships. The third stage consists of the finishing and detailing of the occlusion. In a prospective clinical trial, O’Brien et al2 found that, on average, the total treatment time was 32 months for orthognathic surgery patients, with an average of 25 months for the presurgical phase.
Attempts have been made to reduce the treatment time in adult surgical patients, and one of the possible methods is to eliminate the presurgical orthodontic phase. Few case reports have been published in the literature describing the concept of “surgery first” to decrease the duration of treatment.3-5 Simply through the elimination of the initial decompensation phase, treatment time can be decreased by 9 to 12 months. If an orthodontist uses the “surgery first” approach, the patient does not have to endure the worsening of the soft-tissue profile during treatment. This may result in a paradigm shift in orthognathic surgery to “surgery first orthodontics.”6
The “surgery first” approach also may trigger the regional acceleratory phenomenon (RAP). It may be hypothesized that the osteotomies have a regional effect on the dental osseous environment, possibly resulting in physiologic conditions that are conducive to an accelerated alignment phase after surgery. Since the osteotomies constitute a significant surgical insult, there may be an RAP phenomenon generated that could enhance the speed of tooth movement. However, further research is needed to substantiate this hypothesis.
A precise surgical plan must be based on the tooth inclinations and alignments that the practitioner hopes to achieve after surgery. The surgery can be planned based on the predicted orthodontic movements and the most ideal facial aesthetic outcome. In order to ensure a good occlusal outcome, skeletal anchorage plates are placed during the surgery. These plates allow control following any inaccuracies in surgical outcomes or postsurgical relapse tendencies.
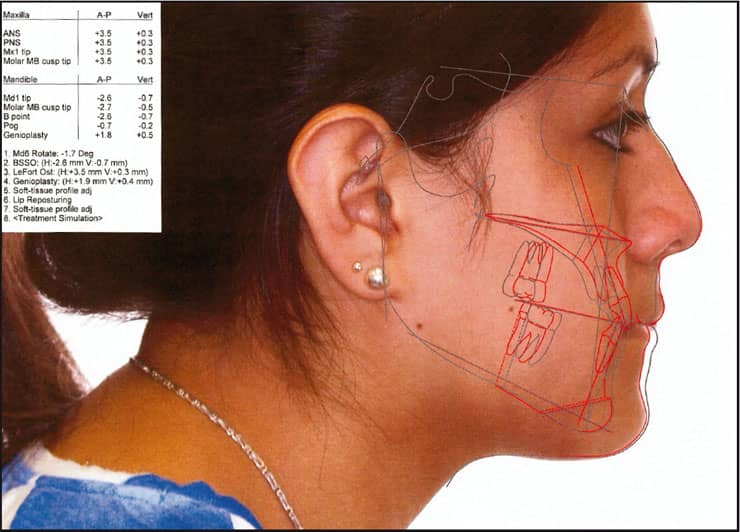
Figure 2A: The surgical plan involved maxillary advancement by 3.5 mm by a Leforte I osteotomy and a 3.5-mm mandibular setback by a bilateral sagittal split osteotomy to finish the patient’s Class I molar and canine.
Case Report

Figure 2B: On the day of surgery, .016 NiTi wires were placed in the maxilla and mandible.

Figure 2C: The patient was discharged from the hospital 1 day after the surgery.

Figure 3: Two months after surgery, the patient had well-aligned upper and lower arches.
A 20-year-old female patient presented a chief complaint that “she did not like her smile.” She had a skeletal Class III malocclusion due to the combination of a retrognathic maxilla and prognathic mandible (Figure 1A). Intraorally, the patient had a full-cusp Class III molar and canine relation bilaterally, with a bilateral posterior and anterior crossbite. There was 4 mm of reverse overjet with 50% deep bite and 4 mm of crowding in the upper and 6 mm of crowding in the lower arch, respectively (Figure 1B). The maxillary and mandibular incisor inclinations were nearly ideal, with 50% incisal display at smile.
The treatment objectives were to correct the underlying skeletal discrepancy to improve the patient’s soft-tissue profile. The surgical plan involved maxillary advancement by 3.5 mm by a Leforte I osteotomy and a 3.5-mm mandibular setback by a bilateral sagittal split osteotomy to finish the patient’s Class I molar and canine (Figure 2A). Additionally, to enhance the soft-tissue profile outcome in the mentolabial fold area, horizontal advancement genioplasty by 2 mm was planned. The crowding in both arches was to be addressed by proximal stripping and mild flaring of the mandibular incisors and 2 mm of distalization of the maxillary left buccal segment using the skeletal anchor plate.
Fixed appliances were bonded 1 week prior to the surgery. On the day of surgery, .016 NiTi wires were placed in the maxilla and mandible (Figure 2B). The maxillary wire bypassed the left canine because space was to be acquired through distalization of the buccal segment prior to bringing the canine into the arch.
After the surgical procedures, the maxilla was stabilized by four plates. In addition, two skeletal anchorage plates were fixed in the infrazygomatic crest. The plates emerged intraorally through the mucogingival junction at the first molar area. The mandible was fixed bilaterally with three bicortical screws and a plate. Skeletal anchorage plates were also used. Short Class III elastics simultaneously settled the patient’s bite. All the third molars were extracted along with the surgery.
The patient was discharged from the hospital 1 day after the surgery (Figure 2C) and was assessed 2 weeks after the surgery. The patient had mild swelling of the face with improved alignment of the arches and settling of the bite. Two months after surgery, the patient had well-aligned upper and lower arches with good facial aesthetics (Figure 3), and 11 months later the patient was debonded after a total treatment time of 13 months. Upper and lower wrap thermoplastic retainers were delivered. Post-treatment pictures (Figure 4) show a significant improvement of the soft-tissue profile as well as a good Class I molar and canine relationship.
Summary
“Surgery first” is a new and innovative procedure for expedited tooth movement in adults. It eliminates the long presurgical phase of orthodontics and possibly uses the RAP phenomenon to increase the rate of tooth movement. However, further research will be needed to validate this claim.

Figure 4: After 13 months of total treatment time, there was significant improvement of the soft-tissue profile as well as a good Class I molar and canine relationship.
Flavio Uribe, DDS, MDentSc, is the program director of the division of orthodontics in the department of craniofacial sciences at the University of Connecticut Health Center. He can be reached at
Aditya Chhibber, BDS, MDS, is a fellow and first-year orthodontic resident at the University of Connecticut Health Center.
Carlos Villegas, DDS, is an assistant professor in the department of orthodontics and maxillofacial surgery at the University of CES in Medellin, Colombia.
References
- O’Brien K. Is early treatment for Class II malocclusion effective? Results from a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2006;129:S64-S65.
- O’Brien K, Wright J, Conboy F, et al. Prospective, multi-center study of the effectiveness of orthodontic/orthognathic surgery care in the United Kingdom. Am J Orthod Dentofacial Orthop. 2009;135: 709-714.
- Sugawara J, Aymach Z, Nagasaka H, Kawamura H, Nanda R. “Surgery first” orthognathics to correct a skeletal Class II malocclusion with an impinging bite. J Clin Orthod. 2010;44: 429-438.
- Villegas C, Uribe F, Sugawara J, Nanda R. Expedited correction of significant dentofacial asymmetry using a “surgery first” approach. J Clin Orthod. 2010;44: 97-103.
- Nagasaka H, Sugawara J, Kawamura H, Nanda R. “Surgery First” skeletal Class III correction using the skeletal anchorage system. J Clin Orthod. 2009;43:97-105.
- Keim RG. The editor’s corner: Surgery-first orthognathics. J Clin Orthod. 2009;43:77-78.








