by Scott G. Smoron, DDS, MSD
How to use a diode laser to set patients up for success
It is easier to achieve ideal orthodontic treatment results when you have achieved ideal orthodontic appliance placement. Teeth with short clinical crowns, slowly erupting teeth, teeth blocked out of the archform, rotated teeth, sites where primary teeth have only recently been lost, altered passive eruption, and stalled eruption due to inadequate space and operculums can all make it difficult to achieve ideal placement of appliances.
Beyond appliance placement, initial gingival architecture is not always aesthetic. Symmetry of clinical crown heights, normal gingival arc shape, and sore or inflamed gingival tissues pose problems for the aesthetic progress and outcome of orthodontic treatment.
By focusing on having more clinical crown available, along with better gingival contours, an orthodontist is more likely to achieve a successful outcome for the patient. Some of the reasons for this success are the following:
- Better hygiene with greater clearance between the appliance and soft tissues. Better hygiene should result in fewer areas of decalcification.
- Fewer appointments needed for repositioning of the appliances.
- More efficient appointments. Powerchains are easier to place when soft tissues do not impinge on the appliances.
- Less breakage as a result of a better bonding field in which gingival crevicular fluid flows further from the adhesive.
- Better overall aesthetics due to improved soft-tissue health and gingival architecture.
- Less pain. Healthier gums equals less inflammation, which equals less soreness.
- Better final dental positions. More visible clinical crown allows better visualization of tooth position. More clinical crown also can equal more success moving teeth with InvisalignTM.
 |
| Patient 1: Several retained primary teeth were removed. Laser surgery then exposes more clinical crown for appliance placement. |
All of the above advantages result from ideal clinical crown availability, which creates the opportunity for patients to succeed with their compliance and achieve more aesthetic and functional treatment results. A simple, $8,000, diode soft-tissue laser gives me the ability to create a path for success by creating ideal clinical crown exposure prior to initiating treatment.
Exposing Clinical Crown on Erupting Teeth
Patient 1 presented with numerous over-retained primary teeth; permanent teeth were visible while primary teeth were still solidly in place. In order to expedite initiation of treatment, the remaining primary teeth were removed. Once the extraction sites healed, I estimated that it would take approximately 6 months for the just-erupting permanent teeth to be ready for appliance placement.
I typically defer treatment on such a patient or initiate treatment with the intent to later add braces as teeth erupt more fully, adding several longer appointments to the treatment plan. Instead, in consultation with the patient and her mother, I decided to use the diode laser and expose more clinical crown. I applied topical anesthetic (a compounded 20% lidocaine, 4% tetracaine, and 2% phenylephrine) to the area to be lased and about 2 mm beyond. The topical was kept in place for approximately 2 minutes and then thoroughly wiped and rinsed away. The tissue was removed uneventfully using 1.2 watts of power on a pulsed mode. Postoperative photos demonstrate a much better clinical picture for appliance placement.
 |
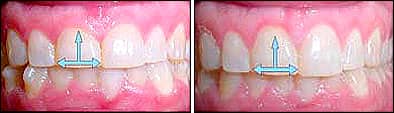
| Patient 2: Asymmetric gingival contours with inadequately exposed clinical crowns. One week post-op photos show clinical crowns ready for appliance placement. Treatment photos 2 months later show placement of appliances on the lateral incisors. |
Improving Gingival Contour
Patient 2 was approaching her 16th birthday. Comparison to previous photos showed that minimal gingival recession was occurring and the clinical crown heights were remaining static. In addition, her gingival margins were asymmetrical, her lateral incisors had inadequate clinical crown, and the left central incisor had an unusual gingival margin contour; instead of an arc, there was a “bump.” Lastly, the labial frenum had been severed in a bicycle accident and had tissue tags remaining. Overall aesthetics were poor.
After discussion, we chose soft tissue lasing to improve the aesthetics and increase the likelihood of quick, efficient orthodontics through ideal appliance placement. I used topical as described for patient 1. I used the laser, again set to 1.2 watts pulsed, to create a better gingival margin on the central incisor and to create symmetry with the other central incisor. I exposed more clinical crown on the lateral incisors as well as the premolars. Finally, I performed a partial frenectomy to clean up the tissue tags. Healing was uneventful, and a week later there was a much better situation for bonding. In-treatment photos show the progress and improved aesthetics of the treatment, along with a strong sense of patriotism (not Patriotism—she’s a Bears fan). Without lasing, I would have expected to reposition at least one bracket, done more wire-bending, and possibly experienced greater breakage as a result of a cluttered bonding field. In addition, the mother immediately was impressed with how much her daughter’s smile improved just from lasing; the smile better reflected her daughter’s age.
Operculum Removal
 |
| Patient 3: Only the mesial cusp tip of this patient’s second molar was erupted. No change was noted for more than 2 years, so the laser was used to remove tissue from the distal half of the second molar’s crown. |
Operculums can prevent incorporation of mandibular second molars into the orthodontic appliance. When second molars are needed, operculum removal can become necessary. Patient 3 presented with a second molar that would not lend itself to banding or bonding. An excellent anesthetic choice for operculum removal is the Oraquix (2.5% lidocaine with 2.5% prilocaine) system. The anesthetic is injected as a liquid through a blunt tip; the liquid turns into a gel once in the gingival crevice or periodontal pocket. The blunt tip resembles a needle, but it does not penetrate tissue. Instead, you place the tip into the central groove on the molar and gently push distally under the operculum, all while pumping the liquid under the tissue. Anesthesia is induced as the liquid/gel makes contact with the soft tissue. Once under the occlusal portion of the operculum, I continue to pump the fluid into the pocket. The fluid then spreads to the distal surface of the tooth and around to the buccal and lingual surfaces of the tooth. Profound anesthesia of the tissue buccal, lingual, occlusal, and distal to the second molar is achieved in a couple of minutes.
I used the laser at a setting of 2.0 watts, in continuous mode, to remove the operculum. I use this higher setting for several reasons. First, the tissue is thicker and more keratinized in some situations, especially to the distal of the molar. Second, the tissues are more thoroughly anesthetized by the spreading of the anesthetic under the tissue. Third, it’s quicker. Within a couple of weeks, there was adequate buccal surface for bonding most appliances, or even banding. In addition, overall hygiene was better without the gingival pocket.
A Partially Erupted Canine
Patient 4 presented with a canine that did not have adequate space to continue eruption. Consequently, it had stalled in place without reaching the occlusal plane. Regular brushing did not produce the normal clinical crown length necessary to properly bond the tooth, and it would not have been prudent to encourage aggressive brushing of a tooth above the occlusal plane due to the risk of tissue loss around the adjacent teeth.
 |
| Patient 4: A partially erupted canine prevented ideal appliance placement. Lasing was performed at initial placement to allow ideal placement. Several months later, without repositioning, the canine is in excellent position. |
Placing a bracket on #11 as it initially presented would have forced me to place a hook-free bracket in a slightly compromised position and hope that hygiene would be excellent. Instead, I chose to set the patient up for success. I applied topical anesthetic for 2 minutes and then removed it; lasing with 1.2 watts in pulsed mode took 1 to 2 minutes.
I bonded this patient’s appliances at the same appointment. In retrospect, more tissue could have been removed to allow better hygiene around the hook of the canine bracket, but the patient did well anyway. In addition, it is better to be conservative. When the first lasing appointment goes smoothly, patients see that the laser is not scary and can produce great results, and they are usually more than willing to repeat the procedure in the future, if necessary.
A Gummy Smile
Patient 5 began Invisalign treatment and was seeing the corrections she had wanted to achieve. However, as we went into the refinement process, the patient and I discussed the poor height/width ratio and resulting “gummy” smile. I also emphasized that the final refinement aligners would be more successful with more clinical crown exposed. In addition, the labial frenum was visible and did not improve the esthetics. I used 2% lidocaine for anesthesia. I lased with 1.2 watts of pulsed power. Once aligner refinement was complete, we planned to consider “touching up” the tissues to improve the arc of the gingival architecture.
 |
| Patient 5: Poor height-to-width ratio resulted in a “gummy” appearance for this aligner patient. A 1-week post-op photo demonstrates a much better height-to-width ratio and a patient thrilled with the less gummy appearance. |
- To read more articles by and about , search for his name in our online archives.
Incorporating laser preparation for bonding into a practice requires planning. Patients who would benefit need to be identified at the initial examination. A detailed discussion about lasing can help allay fears related to pain and/or gum recession. If you do not handle this discussion well, you may scare away new patients. In addition, if it is not planned correctly, lasing can become a separate appointment that delays appliance placement. However, as patients are better identified who could benefit from laser preparation for bonding, the better the treatment results will be in situations that would have typically posed a problem due to the inadequate clinical crowns.
Scott G. Smoron, DDS, MSD, is in private practice in Mount Prospect, Ill. He can be reached at









