More orthodontists are screening patients for sleep disordered breathing than ever, and are treating children earlier in life.
By Kristen Fischer
Orthodontists have become a trusted source for sleep apnea screening and treatment. And many are playing an increased role in screening and treating patients with obstructive sleep apnea (OSA)—namely through oral appliances.
More orthodontists are screening patients for sleep disordered breathing today than in the past—a trend that Mitchell Levine, DMD, who is board certified in dental sleep medicine and orthodontics, thinks will continue.
Levine, a Florida-based associate professor of orthodontics at St. Louis University and president-elect of the American Academy of Dental Sleep Medicine (AADSM), says dentists may provide the first line of screening for most people, as not all people see an orthodontist.
As more graduate orthodontic programs include sleep curriculum, screening will become uniform and widely adopted, he says.
That said, there’s no uniform screening process. “Some provide screening questionnaires and others may start with a question about snoring and see where the conversation may lead,” Levine explains.
Orthodontist Vick Gupta, DDS, MSD, who recently joined Gupta Orthodontics, located in Plano, Tex, says sleep patients comprise up to about 5% of his patients—a number that he expects to grow.
Orthodontists screen and treat patients, but Gupta recommends a sleep study diagnosis from a sleep physician prior to treatment.
“This gives the orthodontist information on the type and severity of sleep apnea. [It] gives the treating doctors a baseline measure so the benefit of the orthodontic intervention can be properly assessed,” Gupta adds.
The American Association of Orthodontists (AAO) recommends prescribing a sleep study before initiating sleep apnea treatment. Orthodontists cannot legally diagnose sleep apnea, Gupta noted. A continuous positive airway pressure (CPAP) prescription is still the top way to treat OSA, but many patients don’t tolerate them well, he adds.
“Many dentists and some orthodontists are treating these patients without a sleep study as it is not ‘required’ to start treatment and can often become an obstacle to getting started,” Gupta points out.
A patient’s care team can include the orthodontist, sleep doctor, ENT, and pediatrician where applicable.
“It is not in the scope of the orthodontist or any other dentist to definitively diagnose obstructive sleep apnea or any other sleep-related breathing disorder,” noted Norman Nagel, DDS, a member of the AAO’s board of trustees.
“Orthodontists can, and should work collaboratively with the physician, to provide orthodontic treatment that could improve OSA in properly selected patients,” Nagel said. A collaborative working relationship with the physician is essential, so the orthodontic treatment does not interfere with medical treatment, he said.
Although orthodontists cannot diagnose and treat obstructive sleep apnea independently, they may be the first healthcare professionals to recognize symptoms in adults and children, Nagel said.
“The specialty of orthodontics involves much more than just moving teeth, and the management of sleep apnea bears witness to this,” Nagel said.
What’s New in Sleep Apnea Treatment
Positive Airway Pressure (PAP) is the gold standard in OSA treatment, but other treatments can be provided for applicable patients via orthodontists.
In terms of what’s new in how orthodontists are treating OSA, it’s become more popular to treat children earlier in life. In addition to oral appliance treatment, maxillary (jaw) expansion is receiving a lot of attention.
“There is mixed evidence to suggest that this approach meaningfully reduces the prevalence of OSA in children,” Levine says.
In adults with narrow maxilla, the concept of hybrid or bone-borne expansion devices has made maxilla expansion a possibility for some who cannot have or do not want surgery.
While there is no question that we can make the maxilla wider, there is limited evidence to suggest that this approach really makes the oropharyngeal airway larger, Levine says.
Clinically, orthodontic thinking suggests making the airway larger will protect the adult or child or reduce the number of events, but that may be at odds with the research that suggests there is limited, if any correlation between airway size and severity of OSA.
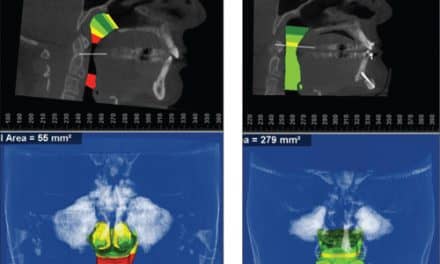
Orthodontists can treat sleep apneas with mild to moderate upper and lower airway obstructions. For upper airway or nasal airway obstructions, they can expand the upper jaw to increase the width of the nasal passages. This is done with an rapid palatal expansion appliance if the patient is still young. For older patients, the orthodontist can utilize an implant supported expander or work with a surgeon for surgically assisted palatal expansion. It’s popular to use anterior mandibular positioning devices for people with lower airway obstructions, Gupta says.
“Although these devices don’t cure the obstruction, they have been shown to provide symptomatic relief for patients when worn during sleep,” Gupta notes.
Research on the benefits of approaches to manage OSA are lagging, Levine says.
Implant-supported expanders—maxillary skeletal expanders (MSEs) or mini implant assisted rapid palatal expanders (MARPEs)—are newer devices that are just starting to be utilized by private practices.
“This device is a great innovation because it allows orthodontist to perform expansion even on those patients who are done growing,” Levine says. They can be effective for males under the age of 30 and for females well into adulthood, and have been effective in expanding the width of the nasal passages and relieving airway or sleep apnea symptoms.
There are also various other products and devices that have been marketed for sleep apnea, but there’s not much solid evidence showing those types of products work well for treating sleep apnea, Gupta says.
Expanding the Orthodontists’ Role
Levine believes the first step to help treat more people with OSA is to let orthodontists screen for it.
“With screening, more prospective patients will be identified. In turn, the orthodontist can make the referral to the appropriate physician for diagnosis,” he adds.
Currently, most orthodontists are referring patients out for treatment of sleep apnea, Gupta says.
“Orthodontists are just starting to become comfortable with the concept of treating sleep symptoms with expanders and repositioning devices,” Gupta says.
With future collaboration between pediatricians, ENTs, and sleep physicians, the role of the orthodontist in treating sleep apnea will only continue to grow, Gupta notes.
“By seeing patients in their pivotal growth years and the recent advances in maxillary expansion, orthodontists are positioned to make a huge positive impact in treating patients with sleep issues,” he adds.
Telemedicine in Orthodontics
Another thing impacting orthodontists is the rise in telemedicine, or teledentistry—especially since the pandemic hit. Levine says it can help reduce the number of certain visits the typical patient may require.
Adjustments may not be required at every visit and as such, the idea of a patient sending in photos or the provider meeting with the patient on a HIPAA-compliant format may allow for fewer in-person appointments. Online visits can reduce missed school or work time, he noted.
“This will work for some parents and adult patients, especially if these are legacy patients,” Levine says.
“On the other hand, some patients really want to see the office, meet the orthodontist, and get a gut feeling on whether a practice is the right place for them,” Levine adds.
Levine thinks patients should see their doctors in person for care, as the basis of care depends on protocol compliance.
“Trust and communication are built on those initial visits,” Levine says. “I think it is valuable for the doctor to help the patient understand why this course of treatment is important. When the patient understands the complexity and cause for concerns, they will more likely adhere to prescriptive treatment.”
Some follow-up appointments could certainly be done remote, especially if treatment is moving forward without any difficulty, he adds.
Nagel added that the AAO has guidance in place to ensure teledentistry is practiced within safe parameters.
Marketing Sleep Care
Levine saw about 35% or more of new patients for sleep-related issues before becoming a full-time faculty member.
When marketing a private practice for sleep-related issues, orthodontists should focus on connecting with local physicians and let them know that orthodontist involvement isn’t about increasing their bottom line.
Many physicians have pre-conceived notions that dentists/orthodontists see sleep as a profit center, Levine says.
“In fairness to physicians, some dentists have given them fuel to foster this thinking,” Levine says. “To that end, the orthodontist should have a sound understanding of sleep medicine—not just the orthodontic devices utilized to manage sleep problems but should be able to converse with physicians in a shared vocabulary.” OP
Kristen Fischer is a freelance writer for Orthodontic Products.