by Gaby Bahri, DDS
An orthodontist tells how he came to adopt this new technology, and how it can help your practice

I remember the time when I left this technique for others to try on their patients and make the mistakes at their own expense; I regret every minute that I spent waiting to start on my first patient. This feeling repeats itself over and over when I hear that in Europe, like in Korea and Japan, microimplants and miniscrews are actually being used routinely by a great number of orthodontists. In fact, those devices are placed and removed by the orthodontist himself. Have you read the article by Melson about this subject?2 For me, the reality was hard to swallow. As Americans, we are not used to taking second place in any field of endeavor, particularly health care. Generally, when we find ourselves in this position, we make sure to put forth the necessary effort to readily change the situation.
Microimplants are the way of the future. Think of them as you think of stop loops, expanders, or torquing appliances. Of course, we can sell them to the patient as an alternative to the most hated of appliances: headgear; but microimplants offer much more than that. Absolute anchorage is the name of the game. It allows you to distalize, mesialize, move individual teeth or groups of teeth, move en masse, move symmetrically or asymmetrically, intrude, extrude, and move impacted teeth. And if you do not want to move all that, fine. Microimplants will serve to just hold everything in place.
Hurdles to Overcome

The second obstacle is becoming convinced of the usefulness of microimplants. In other words, make sure to know what types of cases will yield better results using microimplants. In my experience, outcomes are at least comparable to the best finished treatments using conventional methods, but in shorter time frames.
The third difficulty is in taking the first concrete step toward transforming your practice. Let us not forget the staff. Remember that introducing a new mechanotherapy means pushing your team out of its comfort zone and forcing its members to learn new things. Even though microimplants require some simple, easy training, our staff is a lot like us: They fear the unknown. Once you get your staff involved, though, you will almost certainly be successful in recruiting patients.

The fourth hurdle is learning about the downsides of this method and trying to avoid them. Cost and discomfort are the two most commonly known drawbacks attached to the use of skeletal-anchorage devices. Ensuring that the microimplants are placed in areas close to, or within, the attached gingiva will go a long way to solving both of these problems. Since those areas are very close to the roots of the teeth, the scope of their use is often limited to extraction cases or special cases. Clinicians can argue rightfully that a lot of extraction cases can be treated just as well without the help of the additional anchorage. Although this is true, we have found that the speed with which we can complete treatment still argues in favor of choosing microimplants.
Some extraction cases require more than a conventional anchorage system. As you start to move away from the gingival attachment in an effort to avoid the roots, things get more complicated. The placement and removal of the devices become more involved. Patients will then start to question your new approach to treatment by asking the following questions: Is it really necessary? Can things be done in a different, more comfortable way? What are the expected complications of this intervention? You need to be ready for those questions. For now, all my answers end with the following: “The oral surgeon will give you more accurate details about this procedure.”
Solving Day-to-Day Problems
Once it became established that we use microimplants in my practice, the first growing pains seemed to become more and more remote with time. Now we need to look into solving the day-to-day problems that we all know come with anything in life. Aside from scheduling and mechanics, my personal feeling is that microimplants in orthodontics have two or three major practical problems.
First is the fact that they can loosen up. Failure to hold can happen at the time of placement or at some future time. The second problem is bolting a miniscrew down too close to the bony surface, which means that the head of the screw will be imbedded in soft tissue—which in turn leads to the use of connection devices like chains and plates that emerge from the soft tissues. What normally follows is an inflammatory response around the screws or the connection devices, most commonly around the gold chains we use for traction. Blame it on the patient’s hygiene if you will; but you still have the problem. The third potential problem is the discomfort involved in the activation procedures of the devices. The mechanics are just like those used for impacted teeth; thus, one should pay special attention to the highly sensitive soft tissues surrounding the emerging chain or plate.
Start Small

Offer one or two freebies if that will make you feel better at the beginning. You can do that with a friend on whom you really want to exhibit your best performance. It could be a family member or a referring dentist’s son or daughter. For the rest, it should be clear that the new, added appliances come with a price that is affordable but not cheap. We usually use two screws on the average case. My oral surgeon’s fees are anywhere between $450 and $700 per implant. We can do it for $300 apiece for microscrews and $500 if we are using a bone plate. Orthodontists that place their own implants in the mouth can structure their fees accordingly.
This paper is too short to reveal all the “secrets of the trade,” so to speak, but one can quickly review some of the choices for implants and plates available on the market today. Try to define what exactly it is that you want to accomplish with this new method of anchorage prior to choosing a favorite device. Remember, experience helps.
Here are some general guidelines. Cases in the same category can be treated somewhat similarly:
a) For the maxilla, choose a zygomatic attachment (miniplate or miniscrew) or a microimplant at the level of the gingival attachment.
b) For the mandible, the implant can be placed in the ramus or between the posterior roots (microscrew).
2) Class II cases requiring maxillary molar distalization: Use a zygomatic attachment.
3) Class II cases requiring lower molar protraction: Place microscrews between the anterior/canine roots.
4) Class III cases requiring maximum anchorage for the lower posterior and maxillary protraction forces:
a) Attachments can be placed in the ramus or between the posterior roots in the mandible.
b) Attachments can be placed between the roots of the upper laterals and canines in the maxilla.
Special placement patterns exist for all cases with anterior open bite, deep overbite, asymmetry, mutilated arches and edentulous sections, or impacted teeth.
Common Uses of Microimplants
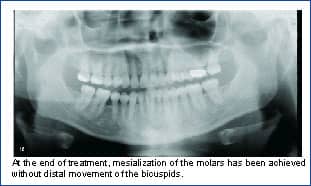
The most common procedure I do is the Class II case with zygomatic implants, followed by bimaxillary protrusive cases using four microimplants at the four corners of the mouth posteriorly. In third position comes the mesial protraction of lower molars.
Retraction cases often exhibit a substantial vertical component that we always have to keep in check. Micro- and mini-implants offer a convenient solution for that problem. Their placement almost always puts them apical to the plane of the archwire; thus, there is always an intrusive component with their use.
In conclusion, the intent of this paper is to bring to the table a hot subject that everyone talks about—yet very little is being done to walk the walk as opposed to talking the talk. I offer these thoughts as an open invitation to American orthodontists to think about the matter. In brief, it will be far better for our patients if we do not drag our feet regarding stepping up and using this new and exciting treatment modality. Future papers will show results and will discuss protocols and mechanics.
Gaby Bahri, DDS, has a private practice in Jacksonville, Fla. He can be reached at [email protected].
References
1. Sugawara J. Dr. Junji Sugawara on the skeletal anchorage system. J Clin Orthod. 1999;33:689–696.
2. Melson B. Mini-implants: where are we? J Clin Orthod. 2005;39:539–547.










