by JOHN W. GRAHAM, DDS, MD, AND JASON B. COPE, DDS, PhD
How to manage potential complications of using temporary anchorage devices
 |
 |
As has been demonstrated in numerous case reports, miniscrew implant (MSI) placement is predictable and stable.1–5 However, implementation of the procedure by clinicians without adequate training in the basic biological and biomechanical fundamentals germane to miniscrews may lead to less-than-ideal treatment results or even complications. The goal of this article is to present potential complications that clinicians may encounter in the routine placement of miniscrews, and how they may be avoided and/or treated.
Inadequate Primary Stability
Primary stability refers to the movement, or the lack thereof, of a miniscrew upon initial placement. A lack of primary stability almost routinely leads to overt miniscrew mobility, with subsequent failure. Recent evidence suggests that the majority of primary miniscrew stability comes from cortical bone, with lesser stability coming from medullary bone.6
Upon placement, a miniscrew should have at least 0.5 mm to 0.75 mm of available bone stock around its circumference. Because most miniscrews are intended to be placed and loaded at the same visit, the miniscrew must have adequate cortical bone purchase and exhibit no mobility.
Another reason for inadequate primary stability is an overdrilled pilot hole.7,8 This problem is more likely in areas of thin cortical bone.9,10 The main reason for hole overenlargement is the clinician’s inability to hold the handpiece stable and perpendicular to the bone surface during drilling. Any lateral movement during drilling will overenlarge the pilot hole.
Excessive trauma during implant surgery is considered an important cause of implant failure.11,12 During a pilot-hole osteotomy, most of the energy not used in the cutting process is transformed into heat. Heat production leading to a temperature rise above 47°C for more than 1 minute negatively affects living bone13 and compromises its regeneration.14 Complications in this area are best avoided by using drill-free screws.
Delayed Mobility
Immediate mobility upon placement also is referred to as inadequate primary stability. Delayed mobility, which occurs days to months after placement, is a separate entity. This type of mobility is usually caused by implant overloading or by underloading.
Implant overloading is caused by force levels applied to the implant that exceed the functional loading capacity of the bone-to-implant interface. Not all mobile miniscrews must be removed. Miniscrews with subtle—not frank—mobility need not be removed. If the miniscrew is stable enough to be loaded by orthodontic forces without frank mobility, it can most likely be left in place.
Static and immediate loading of MSIs stimulates bone formation and the loaded surface, thereby enhancing bone-to-implant contact. Therefore, if a MSI is not loaded immediately, epithelial ingrowth may occur between the bone and the implant, possibly leading to mobility that may worsen with time. Once frank implant mobility is confirmed, the loose miniscrew should be removed and replaced in another location.
Oroantral Communication
During placement of MSIs in the maxilla, there is a chance that the miniscrew might perforate the maxillary sinus. The chance of perforation increases if pneumatization of the sinuses is noted in the preoperative radiographic evaluation. The most concerning sequelae following a sinus perforation are postoperative maxillary sinusitis and formation of a chronic oroantral fistula. The probability that either of these sequelae will occur is related to the size of the communication. If the communication is 2 mm or less, then no further management is required other than routine postoperative observation and sinus precautions.15 Fortunately, this is usually the case, because most current miniscrews are less than 2 mm in diameter.
| Figure 1: Miniscrew placement positions adjacent to tooth roots. |
  |
Temporary Anchorage Periimplantitis
To label infections involving the bone surrounding miniscrews as periimplantitis is a misnomer. Periimplantitis is defined as the pathologic changes confined to the surrounding hard and soft tissues adjacent to an osseointegrated implant.16 The diagnosis of periimplantitis is confirmed by a gradual loss of bone around an osseointegrated implant documented via probing depths and serial radiographs. Because no such osseointegration takes place with most miniscrews, and they are usually removed less than 12 months after initial placement, a term that is more applicable to miniscrews in orthodontics is needed. For the purposes of this discussion, the term temporary anchorage periimplantitis, or TAP, will be used to properly differentiate this phenomenon from true periimplantitis.
Much like periimplantitis, TAP may result from anaerobic bacterial infection at the bone-to-implant interface. Localized bone loss may occur with TAP, resulting in progressive MSI mobility and pain. Radiographic evidence may not be helpful in these situations, given the brief nature of the miniscrew’s role in an orthodontic treatment plan. Because of this, the clinician must identify the potential existence of TAP by clinical evaluation and move forward with the appropriate treatment.
Once identified, a miniscrew that has TAP should be removed. Antibiotic therapy generally is not indicated; however, several days of chlorhexidine rinses should be prescribed to help resolve any associated inflammation.
Tooth-Root Impingement
In a study by Borah and Ashmead17, the incidence of root impingement per screw was 0.47% (13 transfixed teeth per 2,340 screws implanted). Interestingly, none of the impinged teeth developed any documented periapical abscess during follow-up. None of the patients in the study required endodontic treatment or surgical apicoectomy to any of the impinged teeth. The authors concluded, therefore, that tooth-root impingement does not appear to adversely affect tooth survival. A comparable study performed by Fabbroni and colleagues18 yielded similar results.
If the periodontal ligament (PDL) or cementum is contacted, the most frequent concern is that the tooth may undergo ankylosis. Tsukiboshi and colleagues19 suggest that deficits of PDL on the root surface are repaired by new attachment. Andreasen andKristerson20 found that up to 2 mm of PDL loss on the root surface can be repaired by new attachment without ankylosis. Favorably, most current miniscrews are 2 mm or less in diameter.
  |
| Figure 4: Correction of miniscrew attachment-induced soft-tissue trauma. |
  |
| Figure 5: Soft-tissue infection. |
    |
| Figure 6: Miniscrew interference with tooth movement. |
  |
If, during the placement procedure, the clinician does not feel a “drop” into the medullary space as the drill bit or miniscrew continues to advance, the clinician should assume that a tooth root is being encountered. Most commonly, a sign that a root is being contacted is failure of the screw to advance despite adequate pressure. Indication that a root has been contacted mandates redirection away from the root (Figure 1).
Soft-Tissue Injury
Careful attention is sufficient to avoid most soft-tissue injuries. With the vast majority of miniscrew placements, little or no soft-tissue manipulation is required. If a drill-free miniscrew is used, then the clinician inserts the screw through the attached gingiva and manually screws it into the cortical bone without the aid of a drill. This is the simplest method of MSI placement but it requires bone thin enough to facilitate penetration by the MSI alone. Mandibular cortical bone, 3 mm or more thick, may prove in some instances to be too dense to allow drill-free insertion of a miniscrew.
In cases where a miniscrew needs to be placed in a location that is covered by unattached gingiva, it is necessary to utilize a sterile tissue punch to remove the mucosa and periosteum. If a tissue punch is not used, the mucosa has a tendency to wrap around the drill or the miniscrew during insertion, causing needless soft-tissue trauma.
Poor Miniscrew Emergence
Evaluation of the location of the terminal attachment of a miniscrew and its relationship to the desired force vector is critical to a successful outcome. One must also be sure that if a miniscrew is traversing soft tissue, such as in the area of the zygomatic buttress, that the miniscrew is long enough to have both strong cortical engagement and adequate emergence into the oral cavity.
Another aspect of emergence that must be addressed is the local-tissue irritation that a high-profile miniscrew may cause. If the MSI emergence profile is too prominent, then significant irritation to adjacent soft-tissue structures may occur. For example, miniscrews placed between the maxillary lateral incisors and canines for anterior segment intrusion may inadvertently embed themselves in the soft tissue of the upper lip (Figure 2). This situation may be initially treated conservatively with chlorhexidine rinses and liberal application of orthodontic wax, but removal of the miniscrews may be required if the irritation and swelling persist.
Soft-Tissue Impingement
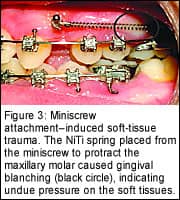
Once biomechanical activation is initiated following the placement of a miniscrew, evaluation of the local soft tissues and their relationships to elastics, open coil springs, and the like is critical. Soft tissues that are adjacent not only to the MSI itself but also to auxiliary mechanical devices are subject to trauma and irritation (Figure 3, page 28). Careful visualization of all soft tissues after active mechanics have been initiated is important to the ultimate success of MSI treatment. For instances in which soft-tissue impingement occurs, auxiliaries such as hooks, arms (Figure 4), or ligatures may be used to redirect or relieve gingival pressure created during miniscrew use.
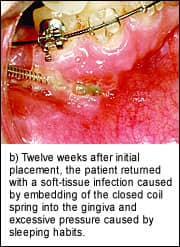
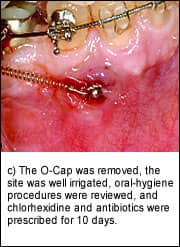
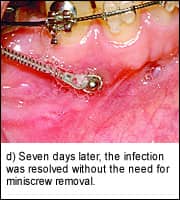
Soft-Tissue Infection
The placement of miniscrews to facilitate orthodontic mechanics requires increased clinical vigilance, specifically in the surveillance of mobility and infection. Fortunately, infections related to miniscrews are easy to recognize and treat. Slight erythema and discomfort immediately adjacent to a miniscrew is the earliest sign of localized infection. If the infection is caught early enough, placing a patient on a regimen of chlorhexidine rinses for 5 to 7 days, along with giving him or her proper hygiene instruction, is sufficient to alleviate most infections (Figure 5). Pus, increasing pain, fever, malaise, and other signs and symptoms of infection indicate the need for a course of antibiotics.
Upon resolution of the active infection, the clinician may choose a suitable alternative location for miniscrew placement and then place a new implant. Added diligence on the part of the orthodontist is necessary for a patient who has experienced a miniscrew-related infection; frequent visits and examinations are prudent in order to avoid further infections.
Undesirable Tooth Movement
A well-thought-out vector analysis is critical to miniscrew success. Unwanted intrusive or extrusive movements are common with miniscrews unless careful attention is paid to vector and force analysis. Molar intrusion may introduce unwanted tipping or crown torque unless proper counterforces are used to prevent such problems.
If, for example, a miniscrew is used in the buccal cortex to intrude a maxillary molar, an opposite force must be placed on the lingual via another miniscrew or a transpalatal arch to prevent unwanted buccal crown torque. Retraction of anterior tooth segments may be subject to intrusive forces or to excessive palatal crown torque. If intrusion is not part of the treatment plan, auxiliaries must be used to place the force vector closer to the center of rotation, thus providing a translational movement of the segment.
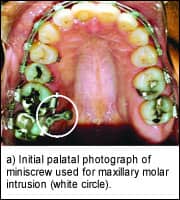
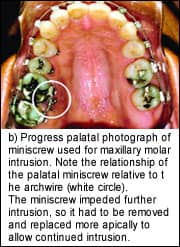
Miniscrew Interference
When miniscrews are used to assist in dental intrusion, it is important to evaluate the anticipated path of the tooth in question. Often, in an attempt to optimally locate a miniscrew for intrusion, the body of the implant is placed directly in the path of the tooth. Progression of the intrusive movement will obviously be arrested, and continued forces on the tooth may contribute to iatrogenic root resorption.
Critical evaluation before miniscrew placement is also necessary to avoid the need for moving the anchor during therapy because of loss of mechanical advantage; for example, not placing a miniscrew far enough away from a tooth to provide ample distance for continuous activation. If a miniscrew is placed too close to a tooth that must be intruded, there may be a point in treatment at which the miniscrew can no longer provide anchorage. In fact, the miniscrew itself may interfere with the mechanics of the movement (Figure 6).
Miniscrew Fracture
Although miniscrew fracture is infrequent, the chance always exists. When the miniscrew fractures at the level of the bone, making removal difficult, it may be appropriate to leave the miniscrew in place. The clinician should choose another site adjacent to the fractured screw and place a new miniscrew. In this instance, a postoperative radiograph will rule out root impingement as the cause for the miniscrew fracture. If the root has been contacted or penetrated by the fractured miniscrew, removal of the remnant is necessary. If the miniscrew is difficult to remove, a small, round bur can be used to create a trough around the exposed miniscrew remnant, allowing adequate access for retrieval.
Postremoval Complications
Postremoval healing complications relate directly to the site of miniscrew removal. If persistent pain, swelling, or drainage occurs after miniscrew-implant removal, chlorhexidine rinses for 5 days will normally resolve any localized infection.
Sinus perforation may not present itself until the miniscrew is removed. If sinus perforation is suspected, the clinician needs to evaluate for the possibility of a fistula. Most likely, if a perforation existed initially, the miniscrew plugged the perforation, and over time the sinus membrane healed over its apex.
Late Complications
Late complications almost exclusively belong to the teeth themselves. Progressive pain and sensitivity to pressure may indicate that a tooth root was penetrated by the TAD and that pulpal damage has ensued. If proper procedures are followed during the planning and placement of miniscrews, this unfortunate circumstance is not likely to go unnoticed until after removal of the miniscrew, but all significant tooth pain in the area of a recent miniscrew removal should be thoroughly investigated.
Because of miniscrews’ small size, ankylosis is rare when using them. As mentioned earlier, PDL breeches of less than 2 mm usually do not progress to ankylosis. If ankylosis is suspected, the clinician should take periapical radiographs to examine the PDL and should perform and document a thorough examination. The clinical relevance of single-tooth ankylosis in an adult is likely minimal, but it should be monitored for internal or external resorption.
Summary
The introduction of temporary skeletal anchorage to the orthodontic world opens up an entirely new era of biomechanics. Naturally, because of the invasive nature of this treatment modality, clinicians may initially hesitate to introduce miniscrews into their routine practice.
There is a paucity of case reports in the literature on complications caused by the placement and use of miniscrews. In the coming years, more case reports and randomized studies will likely demonstrate that the benefits of miniscrews far outweigh the potential risks, thus allowing the orthodontist to expand the horizon of treatment options for all patients.
John W. Graham, DDS, MD, has published several book chapters and journal articles on the use of miniscrews for facial surgery and orthodontics. He lectures and gives in-office courses on miniscrews while maintaining a busy orthodontic practice near Phoenix. He can be reached at [email protected].
Jason B. Cope, DDS, PhD, has a private practice in University Park, Tex. He is an adjunct clinical assistant professor at Baylor College of Dentistry; he has published 18 refereed journal articles, 34 book chapters, and a research handbook; and he has coedited a textbook on distraction osteogenesis. In addition, he has given more than 100 lectures around the world. Currently, he is writing OrthoTADs: The Clinical Guide and Atlas. He is a Diplomate of the American Board of Orthodontics and a member of the Edward H. Angle Society of Orthodontists. He can be reached at [email protected].
This article is excerpted from Graham JW, Cope JB. Potential complications with OrthoTADs: classification, prevention, and treatment. In: Cope JB, ed. OrthoTADs: The Clinical Guide and Atlas. Under Dog Media, LP, Dallas, In Press, March 2006, with permission from Under Dog Media, LP, www.orthotads.com.
References
1. Bae SM, Park HS, Kyung HM, et al. Clinical application of micro-implant anchorage. J Clin Orthod. 2002;36:298–302.
2. Bantleon HP, Bernhart T, Crismani AG, Zachrisson BU. Stable orthodontic anchorage with palatal osseointegrated implants. World J Orthod. 2002;3:109–116.
3. Chung K, Kim S-H, Kook YC. Orthodontic microimplant for distalization of mandibular dentition in Class III correction. Angle Orthod. 2004;75:119–128.
4. Erverdi N, Tosun T, Keles A. A new anchorage site for the treatment of anterior open bite: zygomatic anchorage—case report. J Clin Orthod. 2002;3:147–153.
5. Hong R-K, Heo J-M, Ha Y-K. Lever-arm and mini-implant system for anterior torque control during retraction in lingual orthodontic treatment. Angle Orthod. 2004;75:129-141.
6. Dalstra M, Cattaneo PM, Melsen B. Load transfer of miniscrews for orthodontic anchorage. Orthodontics. 2004;1:53–62.
7. Heidemann W, Gerlach KL, Grobel KH, Kollner HG. Drill free screws: a new form of osteosysthesis. J Craniomaxillofac Surg. 1998;26:163–168.
8. Heidemann W, Terheyden H, Gerlach KL. Analysis of the osseous/metal interface of drill free screws and self-tapping screws. J Craniomaxillofac Surg. 2001;29:69–74.
9. Nunamaker DM, Perren SM. Force measurements in screw fixation. J Biomech. 1976;9:669–675.
10. Phillips JH, Rahn BA. Comparison of compression and torque measurements of self-tapping and pre-tapped screws. Plast Reconstr Surg. 1989;83:447–456.
11. Lundskog J. Heat and bone tissue: an experimental investigation of the thermal properties of bone tissue and threshold level for thermal injury. Scand J Plast Renconstr Surg. 1972;6:5–75.
12. Albrektsson T, Eriksson R. Thermally induced bone necrosis in rabbits: relation to implant failure in humans. Clin Orthop. 1985;195:311–312.
13. Eriksson R, Albreksson T. Temperature threshold level for heat-induced bone tissue injury: a vital-microscope study in the rabbit. J Prosthet Dent. 1983;50:101–107.
14. Thompson H. Effect of drilling into bone. J Oral Surg. 1958;16:22–30.
15. Schow S. Odontogenic diseases of the maxillary sinus. In: Peterson L, Ellis E III, Hupp J, Tucker MR, eds. Contemporary Oral and Maxillofacial Surgery. St Louis: Mosby-Year Book, 1993:465–482.
16. Goldberg M. Control and prevention of infection in the surgical patient. In: Topazian RG, Goldberg MH, Hupp JR, eds. Oral and Maxillofacial Infections. Philadelphia: WB Saunders, 2002:468–483.
17. Borah GL, Ashmead D. The fate of teeth transfixed by osteosynthesis screws. Plast Reconstr Surg. 1996;97:726–729.
18. Fabbronni G, Aabed S, Mizen K, Starr DG. Transalveolar screws and the incidence of dental damage: a prospective study. Int J Oral Maxillofac Surg. 2004;33:442–446.
19. Tsukiboshi M, Asai Y, Nakagawa K, et al. Wound healing in transplantation and replantation. In: Tsukiboshi M, ed. Autotransplantation of Teeth. Tokyo, Japan: Quintessence, 2001:21–56.
20. Andreasen JO, Kristerson L. The effect of limited drying or removal of the periodontal ligament: Periodontal healing after replantation of mature permanent incisors in monkeys. Acta Odontol Scand. 1981;29:1–13.
FIGURES
Figure 1: Miniscrew placement positions adjacent to tooth roots.
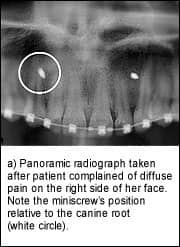
a) Panoramic radiograph taken after patient complained of diffuse pain on the right side of her face. Note miniscrew position relative to the canine root (white circle).
b) Panoramic radiograph taken immediately after removal and redirection of right miniscrew (white circle), which left the patient pain free.









