by Larry M. Wolford, DMD
Can we blame it on the TMJ?

Orthodontic relapse can occur in patients with temporomandibular joint (TMJ) pathologies despite sophisticated treatment. The TMJs are the foundation for jaw position, function, and occlusion. The progressive development of an anterior open bite has commonly been attributed to orthodontic relapse or parafunctional habits such as tongue thrust. However, a common etiology for the progressive development of an anterior open bite is TMJ pathology.
Retruded Mandible
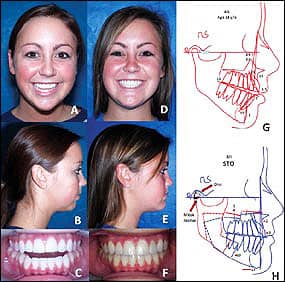
Figure 1: A-C: An 18-year-old with AICR. D-F: 2 years postsurgery for bilateral TMJ disc repositioning and maxillary/mandibular osteotomies. G: A pretreatment cephalogram. H: The surgical procedures advanced the mandible forward 14 mm.
TMJ pathology can adversely affect orthodontic treatment stability, as seen in the 18-year-old female in Figure 1 A–C and G. Her second phase of orthodontic treatment occurred from the age of 12 to 14 with a good occlusion result, but within 6 months after orthodontics she had developed a Class II anterior open bite, TMJ pain, headaches, popping in her TMJs, and difficulty eating. She was placed in a bite splint for 3 years without resolution of her pain and jaw dysfunction prior to referral to the author for definitive treatment.
This is a classic case of Adolescent Internal Condylar Resorption (AICR), one of the most common TMJ conditions seen in teenage females in orthodontic practices. (This conditions occurs in an 8:1 female-to-male ratio). This hormonally mediated condition is initiated as the adolescent enters the pubertal growth phase (between 11 and 15 years). The discs become anteriorly displaced and the condylar heads resorb, with slow but progressive retrusion of the mandible creating a Class II occlusal relation and an anterior open bite. Of these patients with AICR, 25% are asymptomatic relative to pain and joint noises, but still have the displaced discs and condylar resorption. All patients have high occlusal plane angulation with a retruded mandibular facial morphology.
Our treatment protocol has proven to eliminate this TMJ pathology and allow optimal correction of the associated dentofacial deformity. The protocol includes: 1) Remove the reactive tissues surrounding the condyle; 2) reposition and stabilize the disc to the condyle with a Mitek anchor and artificial ligaments; and 3) perform the indicated orthognathic surgery.
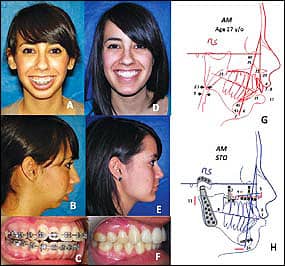
Figure 2: A-C: A 17-year-old with JRA. D-F: 1 year postsurgery for TMJ reconstruction and mandibular advancement with total joint prostheses, maxillary osteotomies, and a chin augmentation. G: A pretreatment cephalogram. H: The surgical treatment advanced the mandible forward 24 mm.
Our studies and others have shown that performing only orthognathic surgery on these patients will result in continued condylar resorption with subsequent skeletal relapse, redevelopment of a Class II anterior open bite, and increased pain. Our protocol has proven to eliminate this TMJ pathology, and produce stable, Class I occlusal outcomes with elimination of pain, improved jaw function, and good facial balance as seen in the presented case (Figure 1D–1F and 1H).
Two additional common TMJ conditions can cause condylar resorption and “orthodontic relapse.” Reactive arthritis (also called seronegative spondyloarthropathy) is an inflammatory process that can occur in the TMJs as a result of bacterial and/or viral pathology. This condition is most commonly seen in females and does not usually begin until the late teenage years or later. Our studies have identified bacteria species from the Chlamydia and Mycoplasma families, but we suspect that other bacteria and viral elements could also be causative factors. These bacteria stimulate the production of substance P, cytokines, and tissue necrosis factor, which are pain modulators. Patients with localized TMJ reactive arthritis may respond well to joint debridement and disc repositioning. In more aggressive forms of the disease, total joint prostheses may be indicated.
Connective tissue autoimmune (CT/AI) diseases, such as juvenile rheumatoid arthritis (JRA), rheumatoid arthritis, psoriatic arthritis, and lupus, can cause severe condylar resorption from reactive tissue within the joints, causing a progressive retrusion of the mandible and a Class II open bite. These conditions can occur at any age, including teenagers or younger. The treatment for these destructive TMJ conditions generally includes bilateral TMJ reconstruction and mandibular advancement with total joint prostheses and maxillary osteotomies.
The 17-year-old female in Figure 2A–2C and 2G was diagnosed with JRA with resultant mandibular retrusion, maxillary anterior vertical hyperplasia, and an anterior open bite). She was treated with our protocol and has a very stable jaw and occlusal relationship, good facial esthetics, and is pain free (Figure 2D–2F and 2H).
Mandibular Prognathism
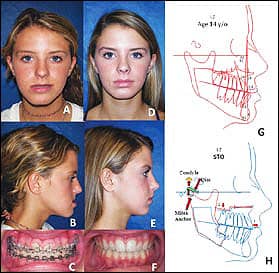
Figure 3: A-C: A 14-year-old with CH Type 1. D-F: 2 years postsurgery for bilateral TMJ high condylectomies, disc repositioning, and maxillary/mandibular osteotomies. G: A pretreatment cephalogram. H: The surgical procedures advanced the maxilla and moved the mandible back.
Overdevelopment of the mandible can also cause orthodontic relapse, as seen in the 14-year-old female diagnosed with Condylar Hyperplasia (CH) Type 1 (Figure 3A–3C and 3G). This condition is caused by an increased growth stimulation of the mandibular condyle, creating accelerated overgrowth of the mandible (prognathism) and a progressively worsening Class III occlusion that can continue to grow into the patient’s mid-20s.
Normal facial and jaw growth is usually 98% complete in females at age 15 and in males at age 17 to 18. CH Type 1 patients may have a Class I occlusion at the beginning of puberty and develop into a Class III or begin as a Class III but develop a worse Class III relationship. Orthodontic mechanics cannot stop or control this abnormal growth mechanism; it can only create significant dental compensations and orthodontic instability. The treatment protocol we developed for these patients includes: 1) Bilateral high condylectomies to arrest the mandibular growth; 2) TMJ disc repositioning on top of the condyles; and 3) simultaneous orthognathic surgery. At 2 years postsurgery, the patient has remained very stable with normal jaw function (Figure 3D–3F and 3H).
Our studies demonstrate that our protocol stops mandibular growth and provides predictable and stable skeletal and occlusal outcomes with normal jaw function and good aesthetics. Treating CH Type 1 with orthodontics and/or orthognathic surgery only, without including the high condylectomies, will result in a high relapse rate with redevelopment of a Class III skeletal and occlusal relationship.
Facial Asymmetry
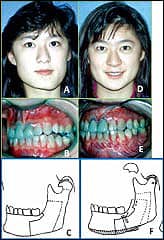
Figure 4: A, B: A 14-year-old with left condylar osteochondroma. D-E: 6 years postsurgery for low condylectomy, maxillary and mandibular osteotomies, and inferior border osteotomy. C and F: The left mandibular procedures are illustrated.
Some TMJ conditions can cause and create progressively worsening facial asymmetry, including the following: 1) Any of the previously mentioned TMJ conditions causing mandibular retrusion (such as AICR, reactive arthritis, CT/AI diseases), if the condition occurs unilaterally or the condylar resorption is more progressive on one side than the other; 2) unilateral CH Type 1 or bilateral with one side growing faster than the other; and 3) CH Type 2, a unilateral overdevelopment (enlargement) of the condyle usually caused by a benign tumor (osteochondroma or osteoma). CH Type 2 will cause unilateral progressive vertical elongation of the mandible and compensatory down-growth of the maxilla. Patients may develop a posterior open bite on the tumor side and a transverse cant in the occlusal plane. CH Type 2 can occur at any age and can be identified radiographically by an enlarged condyle and condylar neck, as well as an increased vertical height of the mandible on the involved side.
The 14-year-old female shown in Figure 4A–4B began developing facial asymmetry at the age of 11 as a result of an osteochondroma of the left mandibular condyle that created vertical elongation of the left side of the jaws and face. The patient was treated according to our protocol and is seen 6 years postsurgery maintaining good stability and normal jaw function (Figure 4D–4E). The treatment protocol we developed to treat this deformity includes: 1) A low condylectomy preserving the condylar neck; 2) recontouring the condylar neck to function as a new condyle; 3) repositioning the articular disc over the new condyle stump; 4) orthognathic surgery; and 5) vertical reduction of the inferior border of the mandible on the tumor side to improve vertical facial balance (Figures 4C and 4F). Our studies have shown that this technique is highly predictable in eliminating the TMJ pathology as well as maintaining long-term occlusal stability and facial balance.
TMD Warning Signs in Orthodontic Patients
Healthy and stable TMJs are necessary for quality treatment outcomes in orthodontics. If the TMJs are not stable and healthy, treatment outcomes for orthodontics may be unsatisfactory relative to function, aesthetics, and occlusal stability. Our recent study evaluated 1,400 TMJ patients referred to the author for treatment. Age range was 8 to 76 years, with 82% females. Interestingly, 70% of the patients reported the onset of the TMJ problems during the teenage years. The orthodontist, therefore, may be seeing many of these patients during their orthodontic treatment.
To read more on this topic, in our online archives.
The orthodontist should be suspicious of possible TMJ problems in the following types of patients: 1) Class II high occlusal plane angle and retruded mandibular morphological type, particularly those with anterior open bites; 2) Class II developing progressively worsening occlusal and jaw relationships; 3) Class III prognathism with progressive worsening; 4) progressive development of facial asymmetry; and 5) patients reporting headaches, TMJ pain, myofascial pain, clicking and popping of the TMJs, and ear symptoms. The orthodontist should not ignore these symptoms! The best results are associated with early recognition and treatment.
With one or more of these symptoms, patients should be evaluated for possible TMJ pathology. An MRI of the TMJs can aid in identification of the specific TMJ pathology. Failure to recognize and treat these conditions can result in significant relapse and a greater complexity of treatment.
Larry M. Wolford, DMD, is clinical professor of oral and maxillofacial surgery at Texas A&M Health Science Center, Baylor College of Dentistry, and is in full-time private practice at Baylor University Medical Center, Dallas. He has written more than 200 articles and book chapters. He can be reached at [email protected].










