by Christopher Piehler
An interview with a pioneer in 3-D craniofacial imaging

OP: What sparked your initial interest in 3-D digital models?
Mah: My original interest in 3-D dental models began when I started my research on creating “Virtual Patients” and I was seeking imaging modalities that provided accurate 3-D information about the patient’s teeth to be used to integrate with other 3-D information about the skeleton and face.
OP: How long have you been working with the technology?
Mah: I started working with 3-D dental models in 1998 when I was using a laser-scanning service to image stone models. Since that time, there have been vast improvements in both scanning technologies and the software to produce high-resolution models. Improvements in overall computer technology, particularly CPU speed and memory capacity, have helped as well.
OP: Do you have any sense of what percentage of orthodontists use 3-D digital models?
Mah: I have to admit that this technology is changing so fast, it is hard for anyone to keep track of the adoption rate. In my conversations with orthodontists, it seems that newer practitioners are gravitating toward 3-D study models for their convenience, portability, competitive cost, and overall “high-tech” value to their practice.
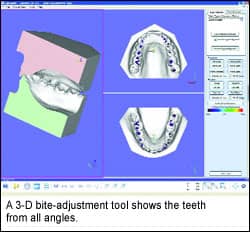
Mah: Indirect methods of creating 3-D models involve imaging of either the impression or the stone model, while direct methods obviate an impression but involve an intraoral camera to image the teeth. An exciting development to watch is the 3-D models that can be produced from a radiographic volumetric image, such as that from a cone-beam CT device (CBCT). Our preliminary studies show that dental arch measurements and analysis for orthodontic diagnosis are just as reliable from the CBCT data. This would also be considered direct dental imaging.
OP: What is the distinction between destructive and nondestructive imaging?
Mah: A method of indirect dental imaging is to photograph or scan the physical dental model before and after a few microns of material are sliced or ground off the model. It takes numerous cycles of scanning and material removal to produce a number of image slices. The slices are then stacked to produce the 3-D model. Nondestructive imaging does not damage the model and is important if the model is to be returned or is part of an archive. Nondestructive imaging can be accomplished by light, laser, infrared, or radiographic means. An advantage of radiographic means is the ability to image in deep crevices, such as those created around severely crowded teeth, where light and lasers cannot penetrate.
OP: In your opinion, what type of modeling is the most accurate and helpful to the orthodontic process?
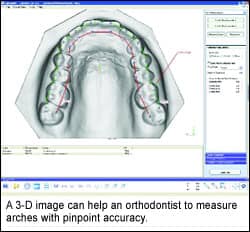
Another aspect of this problem—and, in my opinion, the more important one—is reliability in a clinical situation. It is possible to demonstrate acceptable accuracy of a technology in vitro, but reliability in the mouth is of utmost importance. Challenges such as the wet environment, obstruction of the tongue and cheeks, patient movement, shiny surfaces, and restorations work to decrease performance of the imaging system.
OP: Using 3-D digital models seems to make so much sense. They’re easier to share, and easier to back up. Are there studies that show the impact of using 3-D models on chairtime and treatment outcomes?
Mah: I’m not aware of studies in this regard.
OP: What hardware or software does an orthodontist need to switch to 3-D models?
Mah: Hardware and software are not significant problems. Most common computers can run the software required to view the 3-D models. In addition, commercial providers of 3-D orthodontic study models typically provide the software at no cost.
OP: What costs are involved in the transition, and how much are they offset by the orthodontist’s savings on modeling materials later?
Mah: I believe the costs will be a wash in the beginning, since the costs of 3-D orthodontic study model production is almost the same [as regular model production]. In the long run, the cost savings will come by saving storage space and by management of the models. If physical models need to be produced later, costs will be incurred, but this has not arisen as a significant problem. In fact, companies that produce physical dental models from 3-D data can do so very cost-effectively, at $2–$3 per model.
OP: What standards could professional organizations create that would help guide the use of 3-D models?
Mah: Standards for 3-D orthodontic study models would be a boon for the entire industry, as they would pave the way for both professional and organizational acceptance. This will immediately help sort out the data file formats, interoperability, resolution, and related data-management issues. In addition, one of the barriers to common, widespread acceptance is the concern that the model information is locked in a proprietary format, leaving the orthodontist and patient vulnerable to commercial interests and/or flat-out bankruptcy. At this time, there indeed is an open-member industry-led effort to work with the ADA (ADA SCDI Working Group 11.6) to develop standards.
OP: What else should orthodontists know about 3-D models?
Mah: The current orthodontic study model as we know it is evolving. With 3-D models, manufacturers and techno-orthodontists are pushing the envelope by using this same information for manufacturing of appliances such as aligners and indirect bonding trays. This has produced a need for very accurate impressions or 3-D dental data.
At the same time, 3-D radiographic imaging is rapidly advancing and allowing us to get the same dental arch and tooth-size information as that provided by the traditional stone models. In addition, the radiographic images show the tooth roots, underlying bone, and position of the joints. My prediction for the near future is that the information garnered from traditional stone models will be obtained from the CBCT data, while a high-resolution dental crown data set will be produced for manufacturing purposes.










