by Raphael L. Greenfield, DDS, MScD
An excerpt from the textbook Non Ex Factors: 98.5% Nonextraction treatment Using Coordinated Arch Development

For more than a century, the controversy of treating tooth size/arch length discrepancies, with or without extraction of permanent teeth, has been at the forefront of diagnosis and treatment planning.1-6
So here we are at the beginning of the 21st century, back to a predominantly nonextraction approach—an approach that was discarded 70 years ago. What changes have taken place to influence our profession to such a degree? Certainly, our philosophy of treatment timing has changed radically. Instead of waiting for the completion of second molar eruption and missing the pubertal growth spurt, we generally believe that basal discrepancies are positively impacted when we use the greatest growth increments to our advantage. Beginning in the 1960s, and after encountering significant resistance for almost 15 years, extraoral appliances, such as headgears and functional appliances to temporarily redirect growth, gained widespread popularity and considerable support in the literature.7-16
That said, the management of nonextraction cases has seen the introduction of a plethora of appliances for both maxillary and mandibular (basal) discrepancies. When treating a Class II skeletal discrepancy in a growing patient, the clinician may have to rely on cephalometrics and facial analyses to discern whether a protruded maxilla or retruded mandible is the primary cause. Most cases do not present a clear picture as to which one is the primary cause, especially in a growing patient.
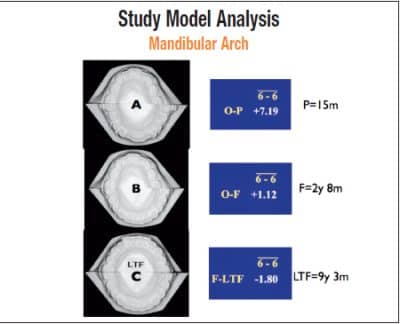
A patient with Class I late mixed dentition was treated with a maxillary removable molar distalizer, mandibular lip bumper, and a cervical headgear worn while sleeping. A) Original intermolar transverse dimension compared to 15 months progress was +7.19 mm. B) Original intermolar transverse dimension compared to final was 7.19 mm + 1.12 mm = 8.31 mm. C) Final intermolar transverse dimension compared to 6 years 7 months post-retention was 8.31 mm – 1.80 mm = 6.51 mm.
Two Class II Approaches
One camp of orthodontists uses mostly mandibular propulsive appliances to reposture the mandible forward and simultaneously redirect maxillary growth.17-22 This philosophy is somewhat similar to Angle’s philosophy more than 100 years ago. In denying the effectiveness of extraoral force, he relied on heavy Class II elastics to favorably influence growth.1 While providing positive orthopedic effects, side effects of this method include a displacement of the anterior teeth labially, which is true with any Class II system. If lower anterior teeth are upright, crowded, or procumbent to begin with, this appliance will further displace these teeth beyond the “neutral zone,” resulting in a significant long-term relapse. If lower incisors are initially recumbent, these appliances can certainly produce a positive result. Therefore, proper case selection is imperative.
Another camp uses extraoral forces such as headgears to redirect maxillary growth and allow mandibular growth to “catch up.”7,8,23 This method, while very effective, relies on patient compliance, and therefore the results will vary. Since the headgear is a maxillary arch appliance, the mandibular incisor position is essentially unaffected. Thus, one could argue that isolating the mandibular arch during Class II skeletal correction may have a positive effect on the long-term stability of mandibular incisor position.
Tooth-Size and Arch-Size Discrepancies
This leads us to the treatment of tooth-size/arch-size discrepancies in the nonextraction case. In extraction treatment, significant crowding is corrected with the removal of permanent dental units—usually bicuspids. However, in the nonextraction case, the deficiency in arch length or arch perimeter is treated with expansion of the arch and/or interproximal reduction. Interproximal reduction is usually relegated to moderate discrepancies (2 mm to 4 mm), while greater discrepancies are treated with expansion.
Types of Expansion
Expansion, according to McNamara,24 can be subdivided into arbitrary categories such as orthodontic, passive, and orthopedic.

Top left are the original intraoral photos. Below that are 15-month progress photos after using only arch-development appliances. The photo at right shows the patient after 12 months of bracket therapy.
“Orthodontic” expansion could also be described as any “mechanical” expansion that employs brackets and archwires, finger springs, removable expansion plates, or quad-helix-type appliances. Generally, these devices tip the crowns labially and the roots lingually. If these movements violate the “neutral zone,” the surrounding musculature may provide an opposing force, leading to long-term relapse.25,59 To help retain the position of the crowns, the roots should be torqued underneath the crowns to establish the forces of occlusion through the long axes of the teeth.

The original occlusal photos of the patient are on top, and the 15-month progress photos are on the bottom.
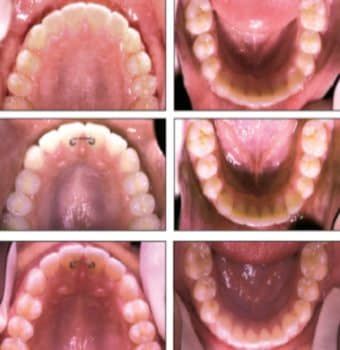
The top two photos show the patient after 2 years and 8 months of treatment. The middle two are the patient 2 years postretention. The bottom two are the patient 6 years and 7 months postretention.

These progress photos show the patient after 15 months of arch development and 15 months of bracket therapy.
“Passive” expansion refers to the blocking of the labial and buccal musculature from the arches. When the orthodontist temporarily removes their influence on the teeth, a widening of the dental arches will frequently occur. This expansion is not produced via biomechanical forces, but rather intrinsic forces such as the tongue. Appliance examples include the lip bumper26,27 and the FrÄnkel appliance.28
“Orthopedic” expansion refers to changes that primarily occur in the underlying skeletal structures rather than the movements of teeth within the alveolus.29-34 Orthopedic expansion not only separates the midpalatal suture, but it also affects the circumzygomatic and circummaxillary sutural systems.35 New bone is deposited at the expansion site within 3 to 6 months to re-establish the integrity of the suture.30

From the top, the final results after 2 years and 8 months of treatment, 2 years postretention, and 6 years and 7 months postretention.

The original photographs (top) contrast with those taken 17 years, 10 months postretention. Retention consisted of a bonded lingual wire between the maxillary central incisors.
Orthopedic expansion, similar to orthodontic expansion, does not directly influence the opposing forces of the surrounding soft-tissue envelope. Thus, the general consensus of the orthodontic community, realizing the possibility of significant relapse, is to “overexpand” the maxilla to almost a complete buccal crossbite. The greatest efficacy of maxillary expansion, at both the skeletal and alveolar levels, is usually during the mixed and adolescent dentitions, prior to the pubertal peak of growth and development.
When comparing rapid maxillary expansion to “slow” maxillary expansion long-term, there were no clinically significant differences in anteroposterior and vertical maxillary changes36 or mandibular behavior.37 One adolescent dentition study initially used rapid maxillary expansion (RME) at one quarter-turn twice a day until the suture was determined to be opened from occlusal films (5 to 7 days). The screw was then turned three times a week until a 2-mm overexpansion was achieved (about 4 months). After evaluating the patient sample about 2½ years after retention, the dental and skeletal changes in the transverse dimension exhibited a high degree of stability.38 Their hypothesis was that slower expansion produced less tissue resistance and stimulated the adaptation process in the circummaxillary structures. These events would minimize any relapse tendency in the long term.
Maxillary expansive forces appear not to be restricted to intermaxillary sutures, but are also distributed to the sphenoid and zygomatic bones and other related structures in the craniofacial complex.39 Histologic studies on animals have also demonstrated signs of increased cellular activity at various cranial sutures.40-44 The available data on suture mechanics appears to have a common theme that mechanical forces regulate sutural growth by inducing sutural mechanical strain. Various orthopedic devices, including headgears, facemasks, and functional appliances, may induce sutural strain, resulting in a modification of natural sutural growth.45,46
Using the effects of expansion on modifying natural, sutural growth, several investigators have applied various headgears for the treatment of skeletal Class II and Class III malocclusions.47-54 Although studies have emphasized the importance of starting earlier in the growth cycle to gain a maximum effect,55-58 there do not appear to be any statistically significant differences between specific entry points in the growth cycle.49 With the exception of one investigation,49 most studies applied the headgears after the rapid maxillary expansion (at two quarter-turns per day) had been completed.47,50-52

The two photos on the left are the original intraoral images. The two on the right were taken 17 years and 10 months postretention.
Coordinated Arch Development Versus Expansion
Coordinated Arch Development® (CAD) is a term I introduced at the 1996 AAO scientific session, together with my partner of 30 years, Jerry Klein, DDS. It is a combined orthopedic/orthodontic approach to long-term stability, applied during periods of optimum growth and development. The approach is based on the following:
- Early treatment of maxillomandibular skeletal discrepancies, preferably in the late mixed dentition. The roots of the “CAD” philosophy are credited to my friend and mentor Norman Cetlin, DMD, of Boston. He emphasized the importance of first molar position over incisor position as the cornerstone of long-term stability. He also preferred the late mixed dentition as the entry point of treatment to utilize “E” space for tooth-size/arch-size discrepancies, when distal movement of first molars could be enhanced by the absence of the unerupted second molars.
- Uprighting upper and lower posterior segments sagittally and transversely, using slow expansion for a greater effect in the same time frame. Uprighting is done in equal increments to prevent the violation of the “neutral zone” during expansion, with the goal of placing the segments well within cancellous bone to allow the optimization of axial inclinations to accept and distribute the functional forces of occlusion through their long axes.
- Controlling the functional occlusal plane by advocating intra-arch mechanics, thereby minimizing the side effects of mechanotherapy.
- Re-educating the intraoral musculature during dimensional changes to the arches by utilizing lip bumpers, inner bows of facebows, and myofunctional therapy when necessary.
CAD distinguishes itself from expansion by the following;
- CAD addresses all three dimensions simultaneously. Expansion focuses on the transverse dimension.
- CAD distalizes the arches during expansion to create a wider dimension of the arch, thereby reducing the amount of necessary expansion. Expansion solely relies on transverse changes.
- CAD coordinates upper arch dimensional changes with lower arch dimensional changes to maximize intercuspation throughout treatment. Maxillary expansion tends to overcorrect the maxillary arch with no corresponding changes in the lower arch.
- CAD attempts to place and maintain the teeth in the “neutral zone” throughout treatment. RME or orthodontic expansion tends to violate the “neutral zone” by placing the teeth into the space of the surrounding musculature. If the musculature cannot adapt to the new transverse dimension, relapse of the teeth toward the “neutral zone” may occur in the long term.
- CAD emphasizes the importance of placing the teeth well within cancellous bone during expansion by slowly and simultaneously expanding and distalizing in relatively equal increments. This allows the integrity of the periodontium to be maintained. In mesially displaced arches (Class II), expanding teeth that have already been placed in areas of narrower cancellous bone could certainly compromise the integrity of the periodontium.
- CAD attempts to “re-educate” the surrounding musculature back to its original resting length by utilizing lip bumpers and the inner bows of facebows. There is no attempt to re-educate the soft tissue envelope in pure expansion.
Raphael L. Greenfield, DDS, MScD, has been in private practice for more than 30 years. He is a diplomate of the American Board of Orthodontics and a referee for the American Journal of Orthodontics and Dentofacial Orthopedics. This article was supported by an educational grant from Ortho Classic. He can be reached at
References
- Angle E. Treatment of malocclusion of the teeth. 7th ed. Philadelphia: SS White Dental Mfg Co; 1907.
- Case CS. The question of extraction in orthodontia. Am J Orthod. 1964;50:658.
- Case, Dewey, and Cryer. The Extraction Debate of 1911. Discussion of Case: The question of extraction in orthodontia. Am J Orthod. 1964;50:751.
- Case, Dewey, and Cryer. The Extraction Debate of 1911. Discussion of Case: The question of extraction in orthodontia. Am J Orthod. 1964;50:843.
- Case, Dewey, and Cryer. The Extraction Debate of 1911. Discussion of Case: The question of extraction in orthodontia. Am J Orthod. 1964;50:862.
- Dewey BF. The Case-Dewey-Cryer extraction debate: A Commentary. Am J Orthod. 1964;50:862-865.
- Poulton DR. Changes in Class II malocclusion with and without occipital headgear-therapy. Angle Orthod. 1959;29:234-250.
- Poulton DR. The influence of extra-oral traction. Am J Orthod. 1967:53:8-18.
- Bernstein L, Ulbrich R, Gianelly A. Orthopedics versus orthodontics in Class II treatment: An implant study. Am J Orthod. 1977;72:549-559.
- Nielsen IL. Facial growth during treatment with the functional regulator appliance. Am J Orthod. 1984;88:401-410.
- Pancherz H. A cephalometric analysis of skeletal and dental changes in contributing to Class II correction in activator treatment. Am J Orthod. 1984;85:125-134.
- Pancherz H, Hagg V. Dentofacial Orthopedics in relation to somatic maturation. Am J Orthod. 1985;88:273-287.
- Ghafari J, Shofer JS, Jacobsson-Hunt U, Markowitz DL, Laster LL. Headgear versus function regulator in the early treatment of Class II division 1 malocclusion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 1998;113:51-61.
- O’Brien KD, Wright J, Conboy F, et al. Effectiveness of early orthodontic treatment with the Twin-block appliance: a multicenter, randomized, controlled trial. Part 1: dental and skeletal effects. Am J Orthod. Dentofacial Orthop. 2003;124:234-243.
- Elms TN, Buschang PH, Alexander RG. Long-term stability of Class II, division 1, nonextraction cervical facebow therapy: Part I. Model analysis. Part II. Cephalometric analysis. Am J Orthod Dentofacial Orthop. 1996;109:271-276,386-392.
- Keeling SD, Wheeler TT, King GJ, et al. Anteroposterior skeletal and dental changes after early Class II treatment with bionators and headgear. Am J Orthod Dentofacial Orthop. 1998;113:40-50.
- Frankel, R. Guidance of eruption without extraction. Trans Europ Orthod Soc. 1971;47:303-315.
- Jacobson A. Jasper jumper color atlas. Am J Orthod. Dentofacial Orthop. 1995;108:341-350.
- McNamara JA. The correction of interarch malocclusion using a fixed force module. Am J Orthod Dentofacial Orthop. 1995;108:641-650.
- Trenouth MJ. Evidence-based orthodontics and the Twin-block appliance. Am J Orthod Dentofacial Orthop. 2002;121:13a-14a.
- Altuna G, Niegel S. Bionators in Class II treatment. J Clin Orthod. 1985;19:185-191.
- Pancherz H. The mechanism of Class II correction and Herbst appliance treatment: a cephalometric investigation. Am J Orthod. 1982;83:104-113.
- Watson W. A computerized appraisal of high-pull headgear. Am J Orthod. 1972;62:561-579.
- McNamara JA, Brudon WL. Orthodontic and Orthopedic Treatment in the Mixed Dentition. Needham Press, 1993.
- Little RM, Riedel RA, Stein A. Mandibular arch length increase during the mixed dentition: postretention evaluation of stability and relapse. Am J Orthod Dentofacial Orthop. 1990;97:393-404.
- Bjerregaard J, Bundgaard AM, Melsen B. The effect of the mandibular lip bumper and maxillary bite plate on tooth movement, occlusion, and space conditions in the lower dental arch. Europ J Orthod. 1983;84:147-155.
- Nevant CT. The effects of lip-bumper therapy on deficient mandibular arch length. Unpublished Master’s Thesis, Department of Orthodontics, Baylor University, Dallas, Texas, 1989.
- FrÄnkel R, FrÄnkel C. Orofacial orthopedics with the function regulator. Munich; S. Karger:1989.
- Haas AJ. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid-palatal suture. Angle Orthod. 1961;31:73-90.
- Haas AJ. Treatment of maxillary deficiency by opening the mid-palatal suture. Angle Orthod. 1965;65:200-217.
- Haas AJ. Palatal expansion: just the beginning of dento-facial orthopedics. Am J Orthod. 1970;57:219-255.
- Haas AJ. Long-term post-treatment evaluation of rapid palatal expansion. Angle Orthod. 1980;50:189-217.
- Timms DJ. Long-term follow-up cases treated by rapid maxillary expansion. Trans Eur Orthod Soc. 1976;211-215.
- Wertz RA. Skeletal and dental changes accompanying rapid mid-palatal suture opening. Am J Orthod. 1970;58:411-466.
- Starnbach H, Bayne D, Cleall J, Subtelny JD. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152-164.
- Filho RMAL, Ruellas ACO. Long-term anteroposterior and vertical maxillary changes in skeletal Class II patients treated with slow and rapid maxillary expansion. Angle Orthod. 2007;77:870-874.
- Filho RMAL, Ruellas ACO. Mandibular behavior with slow and rapid maxillary expansion in skeletal Class II patients. Angle Orthod. 2007;77:625-631.
- Iseri H, Özsoy S. Semi-rapid maxillary expansion: a study of long-term transverse effects in older adolescents and adults. Angle Orthod. 2004;74:71-77.
- Jafari A, Shetty KS, Kumar M. Study of stress distribution and displacement of various craniofacial structures following application of transverse orthopedic forces – a three-dimensional FEM study. Angle Ortho. 2003;73:12-20.
- Gardner GE, Kronman JH. Cranioskeletal displacement caused by rapid palatal expansion in the Rhesus monkey. Am J Orthod. 1971;59:146-155.
- Starnbach H, Bayne D, Cleall J, Subtelny JD. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152-164.
- Starnbach HK, Cleall JF. The effects of splitting the midpalatal suture on the surrounding structures. Am J Orthod. 1964;50:923-924.
- Storey E. Tissue response to the movement of bones. Am J Orthod. 1973;64:229-247.
- Ten Cate AR, Freeman E, Dickinson JB. Sutural Development: structure and its response to rapid expansion. Am J Orthod. 1977;71:622-636.
- Mao JJ, Wang X, Kopher RA. Biomechanics of craniofacial sutures: Orthopedic implications. Angle Orthod. 2003;73:128-135.
- Mao JJ, Oberheim M, Cooper RA, Tassick M. Growth godification. In: McNamara JA Jr, ed. Stress Patterns of Craniofacial Bones Upon Orthopedic Headgear Loading in Dry Human Skulls. Craniofacial Growth Series 35. Ann Arbor, MI: Center for Human Growth and Development, The University of Michigan; 1999:87-104.
- Turley RK. Orthopedic correction of Class III malocclusion with palatal expansion and custom protraction headgear. J Clin Orthod. 1988;22:314-25.
- Campbell RM. The dilemma of Class III treatment. Angle Orthod. 1983;53:175-191.
- Baik HS. Clinical results of the maxillary protraction in Korean children. Am J Orthod Dentofacial Orthop. 1995;108:583-592.
- Fenderson FA, McNamara JA, Baccetti T, Veith CJ. A long-term study on the expansion effects of the cervical-pull facebow with and without rapid maxillary expansion. Angle Orthod. 2003;74:439-449.
- Lima RMA, Lima AL. Case report: long-term outcome of Class II Division 1 malocclusion treated with rapid palatal expansion and cervical traction. Angle Orthod. 2000;70:89-94.
- Turley PEN, Turley PK. Cephalometric effects combined palatal expansion and facemask therapy on Class III malocclusion. Angle Orthod. 1998;68:217-224.
- Irie M, Nakamura S. Orthopedic approach to severe skeletal Class III malocclusion. Am J Orthod. 1977;67:377-392.
- Proffit WR. Contemporary orthodontics. St. Louis: CV Mosby, 1992:237-243, 453-462.
- Dellinger EL. A preliminary study of anterior maxillary displacement. Am J Orthod. 1973;63:509-516.
- Kambara T. Dentofacial changes produced by extraoral forward force in the Macaca irus. Am J Orthod. 1977;71:249-276.
- Nanda R. Biomechanical and clinical considerations of a modified protraction headgear. Am J Orthod. 1980;78:125-139.
- Cozzani G. Extraoral traction and Class III treatment. Am J Orthod. 1981;80:638-650.
- Strang RWH. Fallacy of denture expansion as a treatment procedure. Angle Orthod. 1949;19:12.









