by William (Bill) Harrell, Jr, DMD
Why 3-D imaging is the future of dental diagnostics
Advances in 3-D imaging make 2-D systems practically obsolete. I was the first orthodontist in private practice in the United States to combine a cone-beam dental imaging system and a 3-D facial-capture system to create complete 3-D replications of a patient’s face. As a result, I have first-hand experience in making the technological transition from 2-D to 3-D imaging.
The process gave me a new outlook and a deep appreciation for the predictable outcomes 3-D imaging provides dental professionals and their patients.
The Weaknesses of 2-D Imaging
As we know, the goal of orthodontic diagnosis and treatment planning is to decide the best type and course of treatment. Traditionally, we take 2-D radiographs such as panoramic or lateral cephalometric x-rays and 2-D photographs when a patient requires diagnostic imaging.
In 2-D cephalometric analysis, we average the right and left sides; therefore, we lose bilateral information, an approach that doesn’t take patients’ 3-D soft tissue, bone, tooth structures, and pathologies into account.
Thus, the process of working with 2-D imaging is akin to assembling an abstract puzzle. We take pieces of visual information and try to connect them. We study multiple 2-D images and assemble in our minds an approximation of what our patients’ structures actually look like. From there, we develop our treatment approach.
That has worked for generations, and that was certainly better than working without x-ray imaging at all. But these images have not changed much since they were discovered by Wilhelm Conrad RÖentgen on November 8, 1895, and were later adapted by B. Holly Broadbent, Sr, in 1929 for use in orthodontics with the Broadbent Cephalometer.
2-D imaging machines are certainly higher in resolution and safer today. But they are not the 21st century’s most comprehensive approach to medical imaging. Patients have three dimensions. Medical science operates in three dimensions.
And that’s why working with 3-D images markedly improves the accuracy of diagnosis, treatment planning, monitoring treatment response, and treatment-outcome evaluation. The more precise we are at the outset, the more direct and efficient the process becomes—which can practically eliminate costly or dangerous errors, and reduce adjustments.
Our duty as orthodontic professionals is to use every resource medical science has to offer to provide the most accurate diagnoses and predictable outcomes possible for our patients. That means it is our duty to transition our practices to 3-D imaging sooner rather than later.
 |
 |
The Many Sides of 3-D
And why not? 3-D imaging is, frankly, invaluable. By creating virtual, rotating models that illustrate, in 360º, the complete nature and makeup of the human jaw and face, orthodontic professionals achieve greater accuracy, precision, and efficiency.
3-D imaging provides a more linear path to treatment by taking a complete 3-D scan of the face, displaying the image on a computer screen, and, most important, making it possible for orthodontic professionals to analyze the complete surface.
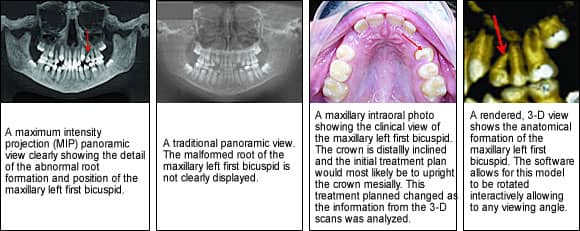
A 3-D scan exposes pathologies and other issues previously undetectable with traditional methods, giving orthodontic professionals a better insight into the relationship between patients’ underlying dental structures and soft tissue—which can lead to discovering the unexpected well in advance of a procedure. In my practice, for example, 3-D imaging reveals anatomically true conditions I never could have discerned with legacy 2-D imaging, such as:
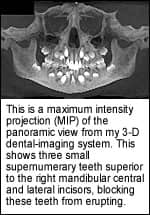
• Impacted teeth. In orthodontics, impacted cuspids are a challenge not only for the surgeon, but also for the orthodontist, who is gaining space and guiding the tooth past adjacent roots into occlusion. 3-D imaging often reveals how the impacted cuspids have already affected surrounding teeth—for example, by shortening the roots. Knowing this information has an obvious impact on the access of the surgical exposure by allowing precise planning of the placement of the attachments by the oral surgeon. 3-D imaging eliminates exploratory surgery for orthodontists and oral surgeons treating both impacted or supernumerary teeth.
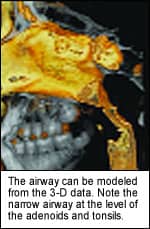
• Airway. Using 3-D imaging helps me find problems related to airway—such as nasal polyps, sinus infections, sinus defects, and tonsil and adenoid impingement on the airway—that I could not have seen easily, if at all, using traditional 2-D techniques. This is especially useful when treating children, as the airway affects their growth and development. Mouth breathing during a child’s growth and development stage has been shown to lead to constricted maxillary arches and long vertical facial pattern (long face syndrome).1-5 With 3-D images on the screen, I can clearly see these conditions and recommend specialists for treatment.
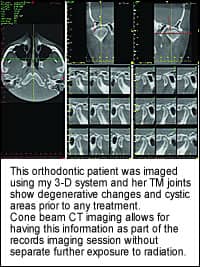
• TMJ. About 15% to 20% of my patients seeking orthodontic treatment, which includes children, have signs and/or symptoms of TMJ before we start treatment. With one scan from a cone beam, I not only have information on the skeletal and dental relationships, but I can also assess the conditions of the TM joints, the airway, and the cervical/spinal area. Deviations on opening can also be documented by taking sequential face images as the patient opens his or her mouth.
• Microimplants. When we consider microimplants for temporary anchorage devices (TAD) to aid orthodontic tooth movement, the cross-sectional images of the microimplant site and the rendered 3-D images help me and the surgeon decide the placement of the TADs that will give the best mechanical advantage for the proposed tooth movement. I can also provide images to the surgeon that show precisely where I want the implants to be, and if they can or cannot fit between the roots of the teeth. The images can be mailed to the surgeon as printed images or through secured e-mail as a PDF file.
Certainly, 3-D’s precision imaging reveals what 2-D never can: the true interrelationships between positions, shapes, and measurements of every facial feature. It is a dynamic connection simply impossible to pinpoint with 2-D x-rays.
Moreover, combining the power of a 3-D radiographic image with a highly precise, color 3-D surface image to create anatomically-accurate 3-D replications of a patient’s face makes treatment more predictable, which improves diagnoses, clarifies surgical approaches, and helps determine appropriate referrals.
 |
 |
Options in 3-D
Moving a practice to 3-D imaging can be challenging. It’s a new and expanding market, with multiple vendors selling fundamentally different 3-D imaging systems. And while some vendors have a long track record, others hung their sign on the door last week. My advice: Understand the basics, and eliminate candidates one by one.
First on any list is cost. Know your budget, and set parameters. Decide how much you’re willing to spend to move your practice to 3-D imaging. Decide which features are crucial and which are unessential. Then try to align real costs with the realities of your requirements. You might find that you have to budget more, or can get away with less. It is your call.
Keep in mind, though, that cost is affected by the equipment’s physical size. It’s crucial to determine early in the process what size device delivers the capabilities your practice needs—and then make certain it will actually fit your available space.
Likewise, consider designs that will be most comfortable for patients. Look for designs that are aesthetically pleasing and minimally intrusive or intimidating. One big plus in this area are systems that offer As Low As Reasonably Available (ALARA) radiation. This ensures that the radiation exposure is sufficient to meet medical requirements, but it does not expose patients to unnecessary levels. While dental-radiation doses tend to be very low, ALARA has added appeal for patients and demonstrates your commitment to patients’ comfort and safety.
Last, investigate software capabilities. Some 3-D imaging systems are doing dazzling things with software, while others are lagging. Build a checklist of software features, and compare each vendor’s software abilities. The differences will be striking.
The Hardware
In the end, I chose the machine with the smallest in-office footprint that produces the most anatomically accurate 3-D views of all oral and maxillofacial structures at the fastest reconstruction time and the smallest, most manageable file size. It was the most practical for my office, my patients, and my work flow. Its’ Extended Field of View option allows me to capture anatomically accurate 22 cm. height scans making it ideal for Cephalometric Reconstruction. It is a 12-bit system, which means it produces images with 4,096 shades of gray. Patients sit in an open environment, which not only increases their comfort, but, most important, captures their full and complete natural anatomical orientation. Data is transferred to an integrated computer—typically, in less than 2 minutes—using small and manageable file sizes. Images are displayed on an intuitive 3-D mapping screen that lets me format and select my desired “slices” for immediate viewing.
To my surprise, the entire workstation—x-ray device, computer station, and access space—requires less than 60 square feet of office space. It images at a reduced cost compared to the other devices I considered, and generates considerably less radiation than traditional fan-beam computed tomography systems.
3-D Imaging Devices and Supporting Software
To complement my highly sophisticated 3-D dental-imaging system, I have also acquired a medically accurate 3-D surface-imaging device that produces highly precise (approximately 0.2 mm) 3-D soft-tissue images of patients’ outer skin and surface features. It does this with no radiation or harmful side effects, and in less than 2 milliseconds. Because the system is noninvasive, I can continuously document, compare, and analyze the patient’s surface topology at every stage throughout the course of the treatment cycle.
I am the first dental specialist in the nation to combine these two technologies to benefit my patients. Pairing images of the outer facial tissue with images of the skull, bone, and teeth lets patients see and better understand the relationship between their dental structure and how it affects their soft tissue or facial appearance. Perhaps best of all, the combination of images conveys changes in facial shape, size, and features resulting from dental treatments. This helps patients feel better educated and more confident when moving forward with treatment plans.
I have further advanced the process by using 3-D imaging software. This program not only transforms the base 3-D images into simple, high-quality, panoramic, lateral, frontal, and submental vertex radiographic projections necessary for orthodontic analysis, but creates 3-D rendered views of the skull, teeth, and soft tissue for 3-D analysis.
The software uses the industry-standard DICOM images to standardize the transfer of information between different medical devices that are manufactured by different vendors with varying digital formats. With that, the software creates linear measurements of both soft tissue and hard tissue points for cephalometric tracings—critical information for any orthodontic specialist.
Better yet, the imaging software combines soft-tissue and hard-tissue images in a composite 3-D display. This visual combination gives me a true, highly precise 3-D view of the outer facial features and tissue of the patient paired with the anatomically accurate 3-D bone imaging, creating a complete diagnostic picture.
Transition Advice
To make the transition from 2-D to 3-D smooth and seamless, and to ensure the best patient outcomes, integrate all your 3-D images at the outset into a single image-management system to streamline workflow processes and consolidate patient data.
Remember that you invested in a 3-D imaging system to make diagnoses more efficient. Do not allow the process to be stymied at the staff level. Hold a thorough training session for all the orthodontists and staff. Make certain everyone understands how to use and gain maximum patient benefit from the technology.
The Role of 3-D
3-D imaging is not only where our profession is heading. It’s where we need to be.
Creating a “virtual patient” gives practitioners the most complete information on the anatomy of a patient’s mouth, face, and jaw areas; and it leads to the most accurate treatment and most predictable outcomes for patients’ surgical procedures.
It directly influences a practice’s overall quality of care. The preoperative scans help dental professionals perform safer, less invasive procedures by increasing precision, thereby reducing risk for the practice and patients. Patients experience far less discomfort afterwards; and they benefit from shorter appointments, faster procedures, more accurate placement, faster recoveries, and cost savings.
For patients, seeing is believing. The visual diagnosis helps communicate their conditions so that they can better understand their treatment options. We are showing them as they exist in nature, with their complete, unique anatomic thumbprint. Embrace the best medical science has to offer: 3-D in-office imaging.
William (Bill) Harrell, Jr, DMD, is board certified by the ABO. He is in private orthodontic practice in Alexander City, Ala, and he also does research in the area of 3-D imaging and TMJ disorders. He has been a member of the AAO Council on Information Technology and is presently serving as the AAO representative to the ADA Standards Committee on Dental Informatics. He can be reached at [email protected].