by Neal D. Kravitz, DMD, MS
Maxillary second molar protraction with mini-implants and a transpalatal arch
When you are protracting maxillary molars, often anterior dental anchorage or Class III directional elastics are sufficient to consolidate space without affecting incisor position. However, in more challenging cases such as movement through a pneumatized sinus or molar substitution, skeletal anchorage may facilitate efficient molar protraction. This case report presents the treatment of an adolescent patient with early loss of dysplastic maxillary first molars and successful, noncompliant protraction of the second molars using orthodontic mini-implants for anchorage.

Figure 1: Pretreatment composite.

Figure 2: Pretreatment cephalograph.

Figure 3: Pretreatment panorex provide by general dentist. Notice the dysplastic first molars (yellow circles).
Diagnosis and Etiology
A 13-year-old adolescent female was referred by her general dentist for an orthodontic consultation following the recent extraction of severely carious maxillary first molars. The patient presented with a straight soft-tissue profile and good facial symmetry, with the maxillary dental midline left of the facial midline. Intraoral examination revealed missing maxillary first molars, full eruption of the maxillary second molars, 180º malrotation of the maxillary left second premolar, forward position of the maxillary right buccal segment due to the labially displaced maxillary right canine, forward position of the left mandibular buccal segment due to lingually displaced mandibular left lateral incisor, and coinciding dental midlines (Figure 1).
As shown in Figure 2, cephalometric analysis confirmed a mild Class II skeletal relationship (SNA: 79º; SNB: 76º). A pretreatment panorex provided by her general dentist revealed large carious lesions with pulpal involvement of the maxillary first molars, presence of all third molars, and acceptable condylar head shape bilaterally (Figure 3).
Study model analysis revealed a Class II division 1 subdivision right malocclusion, a tapered-maxillary arch, 40% overbite, +4 mm of overjet, and moderate anterior crowding.
Treatment Objectives
We identified five treatment objectives:
- establish functional Class I molar and canine occlusion with normal overbite and overjet;
- resolve crowding;
- develop a broader maxillary-arch shape;
- align the dental midlines with the facial midline; and
- maintain soft-tissue esthetics.
Treatment Alternatives
The patient presented to our office with the maxillary first molars already extracted. Therefore, our treatment options were limited to either holding first-molar spaces for restorative treatment or molar substitution (protracting the second molar into the first molar position). The maxillary left second premolar would not be derotated to avoid prolonging treatment duration and risking pulpal necrosis.
In regard to the first treatment option, the maxillary left second premolar would benefit from cuspal coverage; however, no other posterior teeth had carious lesions. Therefore, we did not want to prepare bridgework on healthy teeth. Furthermore, the patient was approximately 4 years from skeletal maturity, and she was not interested in pursuing endosseous dental implants.
The second treatment option included protraction of the maxillary second molars into the first molar position. To aid molar protraction, we discussed incorporating orthodontic mini-implants into the palate. Due to the cost savings and the preservation of healthy teeth, this treatment option was chosen by the patient and supported by her referring dentist.
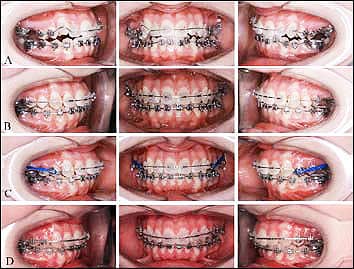
Figure 4: Treatment Montage. A) Upper and lower .014 NiTi wires after bonding. B) Upper and lower .016 x .022 NiTi wires. C) Upper and lower .017 x .025 stainless steel wires. Transpalatal arch has been placed and molar protraction has begun. D) Completion of molar protraction.
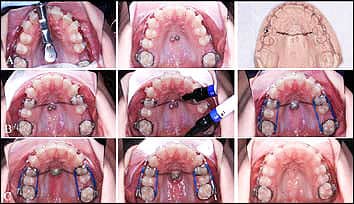
Figure 5: Treatment Montage, occlusal-view. A) Placement of 1.6- x 6.0-mm mini-implants with a torsional-controlled contra-angled driver. Mini-implants placed in the para-medium region. Two mini-implants were placed to stabilize the transpalatal arch. In critique, the mini-implants should have been placed farther apart for greater stability. Pick-up impression taken after placement of the mini-implants. B) We placed flowable composite to secure the transpalatal arch to the mini-implants, and activated molar protraction with buccal and palatal elastic chains. C) Complete consolidation in less than 5 months. Notice the small space opening distal to the right lateral incisor, indicating a slight loss of anchorage even with the skeletal anchorage system.
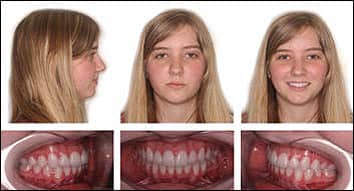
Figure 6: Final composite photographs. Notice the second molars fully protracted into a Class I occlusion. Also notice the lingual cusp of the maxillary left second premolar.
Treatment Progress
We fitted all teeth, excluding the maxillary first premolars, with fixed, preadjusted edgewise appliances (Rocky Mountain Orthodontics Synergy .018 slot in the anterior and Synergy-R .022 self-ligating slot in the posterior. We ligated .014 NiTi aligning archwires (also from RMO). At 2 months of treatment, we switched to .016 x .022 NiTi archwires for anterior torque and arch development (Figure 4).
We placed two RMO Dual-Top mini-implants (6-mm length and 1.6-mm diameter) in the paramedian region of the maxillary palate, in line with the first premolars. We fitted bands on the maxillary first premolars for a pick-up impression to fabricate an AOA Laboratories transpalatal arch spanning premolar-to-premolar. I instructed the laboratory technician to keep the buccal brackets and solder palatal buttons on the bands. After fabrication, we cemented the transpalatal arch with GC Fuji LC, and we added RM Bond flowable composite to secure the mini-implants to the transpalatal bar (Figure 5).
After 4 months of treatment, we inserted .017 x 0.025 stainless steel archwires to begin consolidation. We placed buccal and palatal elastic chains (RMO Medium-Energy Chain) for efficient molar protraction. In less than 5 months (December 2007 to April 2008), we achieved complete space closure with minimal crown tipping.
After 9 months of treatment, we removed the transpalatal arch and mini-implants, then bracketed the maxillary first premolars. We then performed final arch coordination and minimal occlusal equilibration. Once panoramic evidence confirmed mesial migration of the maxillary third molars into the second molar region, we bonded lingual retainers and took impressions for overlay Hawley retainers. At the debonding appointment, we gave the patient a referral for extraction of the mandibular third molars. The total length of treatment was 16 months.
Treatment Results
The results of our treatment were an acceptable Class I relationship and a maintained facial balance (Figure 6). We obtained an appropriate incisal relationship by arch development, distal uprighting of the maxillary anterior teeth, and labial advancement of the mandibular anterior teeth with mild reproximation. Evaluation of pretreatment and posttreatment cephalometric measurements showed significant molar protraction, slight bite opening, and minimal changes in lip position relative to the Esthetic Line (Figure 7).
The 6-month posttreatment records showed good retention of the second molars and continued mesial eruption of the maxillary third molars into the second molar position (Figure 8).
Discussion
Enamel Dysplasia, sometimes referred to as enamel hypoplasia (EH) or simply dysplasia, is a defect that results in underdeveloped or malformed enamel. Dysplasia can occur on any tooth or on multiple teeth, though it most commonly presents on the first molars or the central incisors. The enamel defect may present itself in a variety of forms, from a small pit-lesion to large orange-brownish mottling of the facial or occlusal surface of the tooth. Teeth with enamel dysplasia are often misshapen, hypersensitive, and may be more susceptible to dental caries.1
The cause of dysplasia may be multifactorial, but the defect is most commonly associated with infection or fever during pregnancy or infancy that may interfere with odontogenesis. Other environmental factors may include birth-related trauma to the teeth and jaws, trauma during intubation, poor prenatal and postnatal nutrition (specifically, vitamin A and D deficiency), hypoxia, infections, or exposure to toxic chemicals (such as high dosages of fluoride, tetracycline, and lead). Genetic factors include a variety of hereditary conditions such as trisomy 21, cerebral palsy, and metabolic disorders.1

Figure 7: Superimposition. Maxillary second molars and mandibular first molars were traced.
Treatment options of enamel dysplasia depend on the severity of the lesion. Due to the nature of the dysplastic enamel, bonding is often challenging. Conservative treatment may consist of stainless steel crowns, composite bonding, or root canal with a full-coverage cast crown. In our patient, due to the large carious lesions with pulpal involvement, the general practitioner recommended extraction of the dysplastic first molars followed by protraction of the second molars and spontaneous mesial drift of the third molars.
The literature demonstrates that spontaneous third molar drift following extraction of second molars is highly predicable in the maxilla (96.2%) and less predictable in the mandible (66.2%).2 During eruption, maxillary third molar crowns upright and maintain their angulation as they come into occlusion. Additional uprighting occurs once molar occlusion is established.2 Factors that influence successful third-molar eruption include initial angle of eruption, jaw angulation, sex, age, and developmental stage of the third molar.3 During the treatment of our patient, the maxillary second molars were protracted following extraction of the first molars. A post-treatment panoramic radiograph revealed good erupting position and angulation of the maxillary third molars.
To aid efficient molar protraction, we incorporated indirect skeletal anchorage using an anterior transpalatal arch. Indirect skeletal anchorage is often preferable to direct anchorage when protracting posterior teeth for two reasons:
- greater biomechanical control, because forces are directed along a continuous archwire; and
- greater patient safety, because the mini-implant can be placed in a variety of locations.

Figure 8: The final panorex reveals spontaneous mesial drift of the maxillary third molars into the second molar position. The patient was referred for extraction of the mandibular third molars.
The palate is a preferable location for indirect skeletal anchorage due to its dense cortical bone, attached tissue coverage, and low risk probability.4
With this said, mini-implants were arguably not necessary to aid successful molar protraction in this particular case. It is likely that the depth of pretreatment overbite, with or without the incorporation of a transpalatal arch, would have provided sufficient dental anchorage for molar protraction. While placement of mini-implants ensured anchorage of the transpalatal arch, the benefit of this case report lies in sharing a method for molar protraction that may be more applicable when dental anchorage is insufficient.
Conclusions
Indirect skeletal anchorage with an anterior transpalatal arch can provide efficient, noncompliant maxillary molar protraction. The protraction of maxillary second molars after early loss of first molars, and the subsequent mesial drift of the third molars, allows for the reestablishment of Class I molar occlusion without costly posterior restorative treatment.
Neal D. Kravitz, DMD, MS, is in private practice in South Riding, Va, and White Plains, Md. He is a Diplomate of the American Board of Orthodontics, and is on the faculty at the University of Maryland and Washington Hospital Center. He would like to thank the orthodontic residents at the University of Maryland for their editorial guidance. He can be reached at
References
- Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and Maxillofacial Pathology. 2nd ed. 2002;Philadelphia: W.B. Saunders Company.
- De-la-Rosa-Gay C, Valmaseda Castellón E, Gay-Escoca C. Spontaneous third-molar eruption after second-molar extraction in orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;129:337-344.
- De-la-Rosa-Gay C, Valmaseda Castellón E, Gay-Escoca C. Predictive model of third molar eruption after second molar extraction. Am J Orthod Dentofacial Orthop. 2010;137:346-353.
- Kravitz N, Kusnoto B. Risks and complications of orthodontic miniscrews. Am J Orthod Dentofacial Orthop. 2007;131:S43-S51.










