by Straty Righellis, DDS
A cohort study of consecutively started patients comparing a self-ligating bracket system with traditional twin brackets
 |
Only 18% of the orthodontists in the United States use self-ligating brackets exclusively in treating orthodontic patients.1 While changing bracket systems in an orthodontic office can be disruptive during the transition, when the treatment results are analyzed, the benefits to the patients and the practice can be enormous.
The results of this study support the change from elastomeric ties with twin brackets to self-ligating brackets. The change in bracket systems proved to be positive for both my patients and the practice. The patients benefited from a reduction in chairtime per visit, fewer office visits, and shorter treatment times than originally estimated with conventional, preadjusted, wide twin brackets. The qualitative analysis of the results, using the ABO grading system, showed that using self-ligating brackets produced high-quality treatment outcomes as well.
Self-ligation in general has always made intuitive sense to me. Removing and replacing elastomeric ties is time-consuming. In addition, the force level reduction with elastomeric ties after wire placement is inefficient, requiring frequent patient office visits.2
 |
| Figure 1: The brackets are relatively friction-free with a small, round wire (left). As wire sizes increase (right), earlier interaction helps control inclination and angulation of teeth. |
While there are many self-ligation systems in the marketplace, I selected GAC InOvation R (Figure 1) with its compound contoured base, slot that is in the center of the base,3 and interactive clip.4 This interactive feature allows small wires to work in a relatively friction-free environment during the leveling stages, allowing for rapid tooth movement. As the interactive clip engages into the archwire, control of angulation and inclination of the teeth can be achieved.5 This control is critical for optimal tooth positioning—for example, in an extraction case.
Method and Materials
I used the twin bracket system with elastomeric ties on 88 consecutive patients started in January 1997. The self-ligation sample consisted of 97 consecutive patients started in January 2004. I excluded from the study transfer in/out patients, patients with impacted cuspids, adults, and partial-treatment cases.
Sample similarities included that all cases had the same operator and diagnostic protocol, and used identical bracket prescriptions (.022 Roth Rx with the same bracket slot and base features as in the original Andrews design).
 |
 |
 |
| Figure 2: Before and after 15 visits with four premolar extractions. | Figure 3: Before and after 16 visits with two upper premolar extractions. | Figure 4: Before and after 15 visits without surgery or rapid palatal expansion. |
Figures 2 to 4 are pretreatment and post-treatment photos that demonstrate my goals in tooth positioning for functional occlusion, dento-gingival aesthetics, and facial balance.6–13
I collected the data for treatment efficiency, and Chad R. Sears, DDS, MS independently scored and graded the ABO measurements for treatment outcomes. The grader was calibrated by viewing the instructional DVD produced by the ABO.
Hypothesis
With self-ligating brackets, high-quality treatment outcomes can be maintained with less chairtime, fewer office visits, and shorter treatment times.
Results
On time results: Ninety-one percent of the cases that started were finished “on time.” The nine cases that did not finish on time were delayed either due to second molar impactions (two patients), missing more than five scheduled appointments (three patients), or Class II correction challenges (four patients).
Less chairtime: Our timing studies showed that, in performing a two-archwire change, two people can remove and replace elastomeres in 2 minutes and 38 seconds, while opening and closing the self-ligation clips requires only one person and takes 1 minute and 18 seconds. This results in savings of more than 1 minute per patient per two-archwire change, while using only one staff member to perform the change.14 Furthermore, if the patient is already in finishing wires, no tie removal and reties are needed.
 |
 |
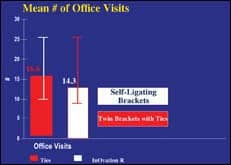
| Figure 5: Using self-ligating brackets meant 2.2 fewer mean office visits. | Figure 6: Self-ligating brackets allowed 24% more cases to be treated without extraction. |
Fewer office visits: Figure 5 shows that using self-ligating brackets required two fewer office visits per active case.
Shorter treatment times: Figure 6 shows a reduction in sample treatment time of approximately 4 months.
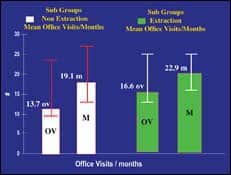
The charts in Figure 7 separate the sample into nonextraction and extraction cases. The nonextraction sub sample, as expected, required fewer office visits and less treatment time.
Figure 8 demonstrates that, in this sample, there was a 24% increase in nonextraction treatment solutions when I used self-ligating brackets.
 |
 |
| Figure 7: Both extraction and nonextraction cases had shorter treatment times with self-ligating brackets. | Figure 8: Cases treated with self-ligating brackets had a mean treatment time of 3.8 fewer months. |
Treatment outcome scores: Forty-five percent of the cases completed with self-ligating brackets scored less than 19 on the ABO Grading System, and another 43% scored between 20 and 25.
The remaining cases that scored greater than 25 usually consisted of diagnoses and treatment plans where dental compensation was planned in patients with underlying skeletal problems—typically Class II correction challenges and anterior open-bite corrections that should ideally be treated with a surgical solution.
The twin bracket group was scored using the Andrews Grading System and got high marks also; however, direct comparison with the ABO grading system would not be valid. A future study is to rescore the twin group using the ABO system.
Discussion
Fewer office visits: With the self-ligation system, the progression from flexible, small, round wires to larger, thermally activated BioForce wires creates a relatively friction-free system. As wire sizes increase, the interactive clips are more efficient than elastomeric ligation because they provide a constant, continuous force that interacts with the archwire for efficient tooth movement between treatment visits.
Shorter treatment times: Previously, cohort studies of my cases over the past 17 years showed that previous diagnostic and treatment protocol changes made in office procedures reduced office visits and improved the quality of the treatment outcomes, but did not reduce chairtime or treatment time significantly.15
The interactive clip feature and the compound contoured bracket system allow for earlier engagement of the wire into the bracket slot for more efficient tooth
movement. Tooth movement can be achieved with the gentle, constant interactive clip mechanism, and the results are of the highest quality in a comparatively short period of time.
Conclusion
Practically, the effects of switching to self-ligating brackets have exceeded my expectations. Over the last 3 years, my annual starts have been constant, but with the reduced chairtime, less frequent office visits, and shorter treatment times, the overall caseload of active patients in treatment has been reduced by 20%. The net effect amounts to 1 less doctor day per month.
While the bracket-system change has been extremely positive, each case still requires a complete and accurate diagnosis with all diagnostic tools available.16–19 Measurable treatment goals for each and every patient must still be the standard in diagnosing and treating our patients.
Further Research to Improve Treatment Efficiency
While this study showed spectacular results, further improvement can be made with changes in wire sizes as we further understand the bracket slot-wire interplay. This study used similar wire sequencing in both samples. We are analyzing ribbon archwires as the spring clip engages earlier in treatment than did the elastomeric ties.
Straty Righellis, DDS, is an associate clinical professor at the University of California at San Francisco. He is a member of the review board of the AJO/DO and a past president of the Northern California Component of the EH Angle Society. He maintains a private practice in Oakland, Calif. He can be reached at
References
- Millennium Research Group. US Markets for Orthodontic Appliances 2007. Available at: [removed]www.mrg.net/TOC_BR/BR_USOD07.pdf[/removed]. Accessed October 22, 2007.
- Thomas S, Sherriff M, Birnie D. A comparison in vitro study of the frictional characteristics of two types of self-ligating brackets and two types of pre-adjusted edgewise brackets tied with elastomeric ligatures. Eur J Orthod. 1998;20(5):589-596.
- Andrews L. Straight Wire: The Concept and Appliance. San Diego: LA Wells Co; 1989.
- Voudouris J. Interactive edgewise mechanisms: form and function comparison with conventional edgewise brackets. Am J Orthod Dentofacial Orthop. 1977;117(3):247-266. Review.
- Thorstenson G, Kusy R. Comparison of resistance to sliding between different self-ligating brackets with 2nd order angulation in the dry and wet states. Am J Orthod Dentofacial Orthop. 2002;121(5):472-482.
- Andrews L. The six keys to normal occlusion. Am J Orthod Dentofacial Orthop. 1972;62(3):296-309.
- Roth RH, Functional occlusion for the orthodontist, Part I. J Clin Orthod. 1981;15(1):32-51.
- Roth RH, Rolfs DA. Functional occlusion for the orthodontist, Part II. J Clin Orthod. 1981;15(2):100-123
- Roth RH, Functional occlusion for the orthodontist, Part III. J Clin Orthod. 1981;15(3);174-198.
- Janzen EK. A balanced smile: a most important treatment objective. Am J Orthod Dentofacial Orthop. 1977;72(4):359-372.
- Rufenacht CR. Fundamentals of Esthetics. Chicago: Quintessence; 1990.
- Moore T, Southard KA, Casko JS, Oian F, Southard TE. Buccal corridors and smile esthetics. Am J Orthod Dentofacial Orthop. 2005;127(2):208-213.
- Hulsey CM. An esthetic evaluation of lip-teeth relationships present in a smile. Am J Orthod Dentofacial Orthop. 1970;57(2):132-144.
- Met Media. InOvation video. Moraga, Calif;2007.
- Jaul D. Treatment changes and treatment efficiency. EH Angle Society Thesis in partial fulfillment for Active Membership, 2004 (unpublished.)
- Shildkraut M, Wood DP, Hunter S. The CR/CO discrepancy and its effect on cephalometric measurements. Angle Orthod. 1994;64(5):333-342.
- Utt TW, Meyers CE Jr, Wierzba TF, Hondrum SO. A 3-dimensional comparison of condylar changes between CR and CO using MPI. Am J Orthod Dentofacial Orthop. 1995;107(3):319-328.
- Wood DP, Korne PH. Centrically related cephalometrics. Am J Orthod Dentofacial Orthop. 1977;71:156-172.
- Wood DP, Elliot EW. Reproducibility of centric relation bite registration techniques. Angle Orthod. 1994;64(3):211-220.










