by JACKIE DORST
Keeping your practice safe means doing more than just following the rules

To make decisions about what needs to be sterilized or disinfected, orthodontists and assistants must be knowledgeable about the Centers for Disease Control and Prevention (CDC) “Infection-control categories of patient-care instruments” laid out in table 4 from the CDC Guidelines for Infection Control in Dental Health Care Settings.1
The CDC Guidelines are the standard of instrument reprocessing and infection control under most state dental-practice acts. However, some states may have even more rigorous or more specific infection-control requirements.
Sterilization VersusDisinfection
Using inappropriate sterilization or disinfection techniques can put patient safety at risk, damage patient-care items, and result in clinical-team inefficiency and frustration. The CDC defines sterilization and disinfection in the following manner:
Sterilization: The use of a physical or chemical procedure to destroy all microorganisms, including substantial numbers of bacterial spores.
Disinfection: The destruction of pathogenic and other kinds of microorganisms by physical or chemical means. Disinfection is less lethal than sterilization, because it destroys the majority of recognized pathogenic microorganisms but not necessarily all microbial forms (such as bacterial spores). Disinfection does not ensure the degree of safety associated with sterilization processes.
It is important that the entire clinical team understands the difference between sterilization and disinfection. According to the definition of disinfection, “Disinfection does not ensure the degree of safety associated with sterilization processes.”
Based on this definition, it is understandable why the CDC Guidelines state that disinfection is appropriate only for noncritical patient-care items such as curing lights, exam lights, and extraoral cameras. These items can be cleaned and disinfected with a low- to intermediate-level disinfectant, or can be used with a removable barrier.
Noncritical items contact only intact skin, and therefore have a lower risk of disease transmission than critical or semicritical items. Noncritical items should be cleaned to remove any saliva, blood, aerosols, or body fluids, then disinfected with a hospital disinfectant registered with the Environmental Protection Agency. All contaminated surfaces must be cleaned before disinfection. If the surface is contaminated with saliva, debris, or other potentially infectious material, the disinfectant will not be effective.

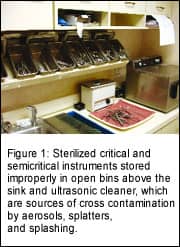
Critical and semicritical items, which have the greatest potential to transmit disease, should be cleaned and heat sterilized. These items should also be packaged in pouches or wraps before sterilization to prevent recontamination if they will not be used immediately after sterilization.
Critical patient-care items—those that penetrate soft tissue or bone—in an orthodontic practice include scalers, explorers, and band pushers. Semicritical items—those that touch mucous membranes or nonintact skin—include orthodontic pliers, cheek retractors, impression trays, and mouth mirrors.
Sterilization Methods
Critical and semicritical items that are heat sensitive—meaning that they will be damaged or destroyed during heat sterilization—can be processed by cleaning them with a sterilant/high-level disinfectant cleared by the US Food and Drug Administration, closely following the manufacturer’s instructions. After the items are soaked for the required length of time, they must be rinsed with sterile water—not tap water. Tap water can contain up to 500 CFU/ml of microoganisms, which will recontaminate the items.
It is very difficult and costly for orthodontic practices to rinse items with sterile water. Also, chemical sterilants, commonly called “cold sterilization,” are highly toxic and require safety precautions. For this reason, I recommend that all my clients use autoclaves for handpieces, cheek retractors, and elastomeric ligatures. Autoclaves sterilize at lower temperatures (between 250°F and 273°F) than dry-heat sterilizers, which reach temperatures of 375°F or greater. Using one method of sterilization for all items improves efficiency and reduces errors that can compromise patient safety and damage expensive instruments. Having three different systems such as dry heat, chemical sterilant, and autoclaves requires time-consuming sorting of items and increases the risk of damaging instruments by accidentally placing an instrument in the wrong sterilization system.
Safety in Numbers

1) knowledgeable clinical team members;
2) proper equipment and space; and
3) adequate instrument inventory for the recycle time.
Orthodontic practices that meet these three instrument-reprocessing requirements ensure that every patient visit is safe from the risk of disease transmission. Efficient, standardized systems for instrument reprocessing reduce stress for the clinical team and provide patients with the visual reassurance of the cleanliness and safety of the practice.
The current CDC Guidelines provide the standard of care for instrument reprocessing and infection control for all dental practices in the United States, including orthodontists. What I have learned from my orthodontic clients, though, is that the methods for sterilization and disinfection are not just about meeting the rules and regulations of their respective state dental boards and the Occupational Safety and Health Administration. Sterilization and cleanliness also affect patients’ and parents’ perceptions of the orthodontic practice. New orthodontic patients and parents can be positively influenced about the quality of the practice after touring the clinical area and viewing the systems for reprocessing patient-care items.
Orthodontic patients and parents today are more aware than in the past of the risks for disease transmission in health care and public areas. The media reports daily on the spread of avian flu, water contamination, and infections among cruise ship passengers. The orthodontic clinical team can reassure patients that they understand the CDC Guidelines and practice proper sterilization and infection-control care in a clean, safe environment. Team members should enthusiastically discuss with patients all the steps taken to ensure that every orthodontic visit is a safe one.
Orthodontic teams should understand the instrument categories so that they can determine how to properly clean, sterilize, or disinfect all patient-care items. Educating the clinical team prevents oversterilization and understerilization, and ensures patient safety. Invest time in your team training and equipment so that your practice reprocesses patient-care items efficiently and effectively.
Jackie Dorst is a speaker and consultant on orthodontic sterilization design, infection control, and safety. As a microbiologist and dental hygienist,she combines science with practical clinical applications for orthodontic efficiency and safe patient care. She is a frequent speaker at AAO national and component meetings. She can be reached at (904) 206-4361 or [email protected].
Reference
1. Kohn WG, Collins AS, Cleveland JC, Harte JA, Eklund KJ, Malvitz DM. Centers for Disease Control and Prevention (CDC). Guidelines for infection control in dental health-care settings—2003. MMWR Recomm Rep. 2003;52(RR-17):1–61.